The axilla, also known as the armpit, serves as a critical transition zone between the upper limb and the thorax, and understanding its boundaries is paramount for clinicians. Specifically, the walls of axilla, defined by various muscles and the scapula, create this pyramidal space. Careful examination of these walls of axilla is essential during procedures such as axillary lymph node dissection, a common intervention for managing breast cancer. The meticulous anatomical knowledge of these walls of axilla helps in accurate diagnosis and treatment planning, benefiting both the physician and the patient.
The axilla, more commonly known as the armpit, is far more than just a surface landmark. It represents a complex anatomical region serving as a crucial crossroads for neurovascular structures supplying the upper limb. Comprehending the axilla’s intricate anatomy, particularly the formation and contents of its walls, is of paramount importance in clinical practice.
The Axilla: A Vital Anatomical Hub
The axilla is a pyramidal space situated between the upper limb and the chest. Its location is strategically vital, acting as a conduit for major blood vessels, nerves, and lymphatic vessels traversing between the trunk and the upper extremity.
This region’s boundaries are well-defined, forming distinct walls that encapsulate and protect these essential structures. Understanding these walls is fundamental to accurately diagnosing and treating a wide range of conditions.
Clinical Significance: Why the Axilla Matters
The axillary region holds significant clinical relevance for several reasons:
-
Vascular Access: The axillary artery and vein, critical components of the circulatory system, are readily accessible within the axilla. This accessibility makes the region a common site for vascular access, diagnostic procedures, and surgical interventions.
-
Nerve Blocks: The brachial plexus, responsible for innervating the entire upper limb, courses through the axilla. Anesthesiologists frequently utilize the axilla to perform nerve blocks, providing targeted pain relief or anesthesia for upper extremity procedures.
-
Lymph Node Involvement: The axilla houses a dense network of lymph nodes. These nodes play a vital role in immune surveillance and lymphatic drainage. However, they are also common sites for metastasis, particularly in cases of breast cancer. Palpation and assessment of axillary lymph nodes are thus crucial in cancer staging and treatment planning.
-
Injury Vulnerability: Due to its location and the concentration of vital structures, the axilla is susceptible to injury from trauma, compression, or surgical procedures. A thorough understanding of the regional anatomy is essential to minimize the risk of iatrogenic damage.
Exploring the Landscape: Purpose and Scope
This article aims to provide a comprehensive overview of the axilla. We will delve into the anatomical intricacies of its walls, exploring their composition, muscular attachments, and associated neurovascular structures.
Furthermore, we will discuss the clinical significance of the axillary region, highlighting common pathologies, diagnostic considerations, and surgical approaches.
By synthesizing anatomical knowledge with clinical applications, this article aims to equip healthcare professionals and students with a deeper understanding of the axilla and its importance in clinical practice.
The axillary region holds significant clinical relevance for several reasons, including its accessibility for vascular access, its use in nerve blocks, and its importance in lymphatic drainage and the spread of cancer. But before delving into specific clinical scenarios or the intricacies of each wall, it’s crucial to establish a solid foundation in the axilla’s fundamental anatomy.
Anatomical Foundation: Defining the Axillary Space
The axilla, often referred to as the armpit, is more than just a surface feature; it’s a complex three-dimensional space. Understanding its boundaries, shape, and contents is essential for comprehending its role in upper limb function and related pathologies.
Demarcating the Boundaries of the Axilla
The axilla is best understood by defining its six boundaries: the apex, base, and four walls (anterior, posterior, medial, and lateral). Each of these boundaries is formed by specific anatomical structures that contribute to the overall shape and function of the axilla.
-
Apex (Axillary Inlet): The apex, or inlet, of the axilla is the superior opening that connects the axilla to the neck. It is bounded by the clavicle anteriorly, the superior border of the scapula posteriorly, and the outer border of the first rib medially. Through this apex, the neurovascular structures supplying the upper limb enter the axilla.
-
Base (Axillary Floor): The base of the axilla is the inferior boundary, formed by the axillary fascia and skin stretching between the lower borders of the pectoralis major and latissimus dorsi muscles. In simpler terms, it’s the skin and tissue you feel when you palpate your armpit.
-
Anterior Wall: This wall is primarily formed by the pectoralis major and minor muscles, along with the associated clavipectoral fascia. It essentially forms the front of the armpit.
-
Posterior Wall: Composed of the scapula, subscapularis, latissimus dorsi, and teres major muscles, the posterior wall creates the back boundary of the axilla.
-
Medial Wall: The medial wall is made up of the serratus anterior muscle and the thoracic wall (ribs 1-4 and the intercostal muscles). This wall is closest to the midline of the body.
-
Lateral Wall: The lateral wall is the narrowest of all the walls, and it is formed by the intertubercular groove (bicipital groove) of the humerus.
Shape and Dimensions: A Pyramidal Space
The axilla is characteristically pyramidal in shape, with its apex pointing towards the root of the neck and its base oriented inferiorly. The dimensions of the axilla vary from person to person, depending on factors such as body size and muscle development. However, it’s generally agreed that the lateral wall represents the narrowest point in the axillary space.
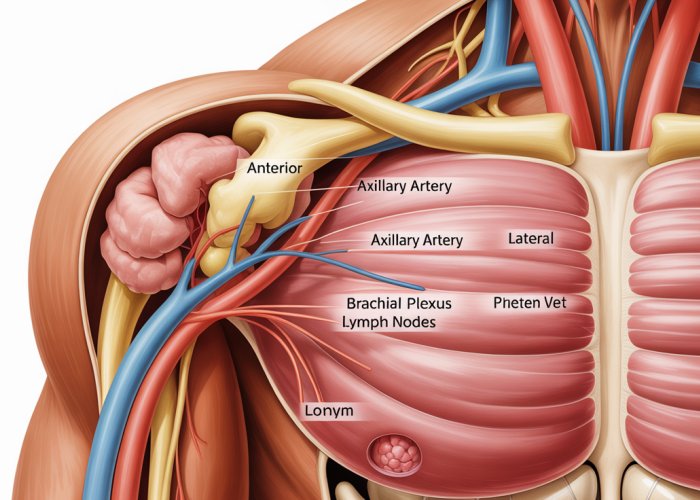
Contents of the Axilla: A Neurovascular Hub
Within the boundaries of the axilla lies a collection of critical anatomical structures, including:
-
Blood Vessels: The axillary artery and its branches supply blood to the upper limb, while the axillary vein and its tributaries drain blood from the upper limb. These vessels are the lifeline of the arm and hand.
-
Nerves: The brachial plexus, a complex network of nerves, provides motor and sensory innervation to the entire upper limb. Damage to this plexus can result in significant functional impairment.
-
Lymph Nodes: A network of axillary lymph nodes plays a vital role in immune surveillance and lymphatic drainage of the upper limb and the breast. These nodes are often involved in the spread of cancer.
-
Muscles: Portions of several muscles, such as the biceps brachii and coracobrachialis, also reside within the axilla or contribute to its boundaries.
By understanding the boundaries, shape, and contents of the axilla, clinicians and students can develop a robust framework for further exploration of this vital anatomical region. The upcoming sections will delve into each wall in greater detail, revealing their specific composition and clinical relevance.
The Anterior Wall: Pectoralis Major and More
With the foundational understanding of the axillary space now established, it’s time to explore the intricate details of its boundaries. The walls of the axilla are not mere borders, but rather complex anatomical landscapes, each with its own unique composition and clinical significance. We begin our journey with the anterior wall, a region dominated by the powerful pectoralis major muscle.
Defining the Anterior Boundary
The anterior wall of the axilla is primarily formed by the pectoralis major muscle, a large, fan-shaped muscle that covers much of the anterior chest wall.
However, the anterior wall is not solely composed of muscle.
The clavicle, along with the clavipectoral fascia, also contributes to its structure, particularly in the superior aspect.
This fascia, a layer of connective tissue, lies deep to the pectoralis major and envelops the pectoralis minor and subclavius muscles.
Pectoralis Major: Attachments and Action
A thorough understanding of the pectoralis major muscle is essential for appreciating the anatomy of the anterior wall.
This muscle plays a crucial role in the movement of the upper limb, particularly in adduction, flexion, and internal rotation of the humerus.
Origins and Insertions
The pectoralis major has a broad origin, arising from the clavicle (clavicular head), the sternum, the costal cartilages of ribs 1-6 or 7, and the aponeurosis of the external oblique muscle.
This extensive origin allows the muscle to exert its force across a wide range of movements.
The muscle fibers converge to insert onto the lateral lip of the intertubercular groove of the humerus.
This insertion point allows the pectoralis major to effectively act on the humerus, controlling its movement in various planes.
Functional Significance
Contraction of the pectoralis major muscle results in adduction, flexion, and internal rotation of the arm at the shoulder joint.
It also assists in deep inspiration by elevating the rib cage when the arm is fixed.
The muscle’s dual origin allows for differential activation of the clavicular and sternocostal heads, enabling more refined control of arm movements.
Neurovascular Structures of the Anterior Wall
Several important neurovascular structures traverse or are closely related to the anterior wall of the axilla.
These structures are essential for the function and innervation of the upper limb and chest wall.
Pectoral Nerves
The medial and lateral pectoral nerves are key to innervating the muscles of the anterior wall.
The lateral pectoral nerve pierces the clavipectoral fascia to supply the pectoralis major, while the medial pectoral nerve pierces the pectoralis minor to supply both the pectoralis minor and pectoralis major.
These nerves carry motor signals to control muscle contraction and movement.
Thoracoacromial Artery and Vein
The thoracoacromial artery, a branch of the axillary artery, pierces the clavipectoral fascia to supply the pectoral region, as well as the acromion and shoulder region.
It has several branches, including the pectoral, acromial, clavicular, and deltoid branches.
The thoracoacromial vein drains blood from the same regions, eventually emptying into the axillary vein.
Clinical Considerations
The anterior wall is clinically relevant in several ways.
For example, surgical procedures involving the breast, such as mastectomy, may require careful dissection of the pectoralis major muscle and its associated neurovascular structures.
Knowledge of the anatomy of the anterior wall is also essential for performing pectoral nerve blocks, which are used to provide pain relief following surgery or trauma to the chest wall or upper limb.
Understanding the anatomy of the anterior wall, including the pectoralis major muscle, clavicle, associated fascia, and neurovascular structures, is crucial for clinicians and anatomists alike. This knowledge forms the basis for comprehending the function and potential pathologies of this important region.
The anterior wall, with its powerful pectoralis major, provides a strong shield and anchor for upper limb movement. But what lies behind this prominent structure? Moving posteriorly, we encounter a different landscape, one sculpted by the scapula and a collection of muscles that orchestrate the complex movements of the shoulder. The posterior wall of the axilla offers a critical foundation for the glenohumeral joint and provides pathways for vital neurovascular structures.
The Posterior Wall: Muscles of the Shoulder
The posterior wall of the axilla is a robust structure primarily formed by the scapula and the muscles that overlay it, namely the subscapularis, latissimus dorsi, and teres major. These muscles, each with distinct origins, insertions, and actions, work synergistically to provide stability and a wide range of motion to the shoulder joint. Understanding their individual contributions is paramount to appreciating the functionality of the posterior axillary wall.
Defining the Posterior Boundary
The formation of the posterior wall is a layered affair.
-
The Subscapularis Muscle: This muscle occupies the subscapular fossa on the anterior surface of the scapula, forming the upper portion of the wall.
-
The Scapula: The bone itself serves as the foundational structure.
-
Latissimus Dorsi and Teres Major Muscles: These muscles ascend from the inferior angle of the scapula, contributing to the lower portion of the posterior wall.
The long head of the triceps brachii also passes through this area.
Muscle Attachments: Origins and Insertions
A detailed understanding of the origins and insertions of these muscles is crucial to appreciating their function.
Subscapularis
-
Origin: The subscapularis originates from the subscapular fossa, a large concave depression on the anterior surface of the scapula.
This broad origin provides a strong base for its actions. -
Insertion: The muscle fibers converge to insert on the lesser tubercle of the humerus.
This insertion point makes it a primary internal rotator of the arm.
Latissimus Dorsi
-
Origin: The latissimus dorsi has a vast origin, arising from the spinous processes of vertebrae T7-L5, the thoracolumbar fascia, the iliac crest, and the lower three or four ribs.
This extensive origin underscores its role as a powerful mover of the upper limb and trunk.
-
Insertion: The muscle spirals around the teres major to insert into the intertubercular groove of the humerus.
This insertion allows it to adduct, internally rotate, and extend the arm.
Teres Major
-
Origin: The teres major originates from the inferior angle of the scapula.
-
Insertion: It inserts onto the crest of the lesser tubercle of the humerus, just anterior to the latissimus dorsi insertion.
This close proximity and similar line of pull mean it often acts synergistically with the latissimus dorsi.
It assists in adduction and internal rotation of the arm.
Neurovascular Structures of the Posterior Wall
The posterior wall is not merely a muscular barrier; it also serves as a conduit for essential neurovascular structures supplying the upper limb.
Understanding these relationships is vital for preventing iatrogenic injury.
-
The Subscapular Artery and Vein: These vessels run along the inferior border of the subscapularis muscle, providing blood supply to the scapular region and surrounding muscles.
The subscapular artery is the largest branch of the axillary artery. -
The Thoracodorsal Nerve: This nerve, a branch of the posterior cord of the brachial plexus, innervates the latissimus dorsi muscle.
It runs with the thoracodorsal artery. -
The Axillary Nerve: While primarily associated with the surgical neck of the humerus, the axillary nerve courses near the upper aspect of the posterior wall as it exits the axilla.
It innervates the deltoid and teres minor muscles. -
The Radial Nerve: The radial nerve passes inferior to the teres major.
Damage to these nerves can result in significant functional deficits in the upper limb. The structures passing through the quadrangular space are especially vulnerable to injury.
The posterior wall, therefore, is a complex and clinically significant region. It stabilizes the shoulder and acts as a vital pathway. A thorough understanding of its anatomy is crucial for clinicians managing shoulder pathology and performing surgical procedures in the axillary region.
The muscles of the posterior wall create a dynamic interface with the humerus and shoulder joint. Now, shifting our attention medially, we encounter the wall defined by the rib cage and a powerful muscle that secures the scapula: the serratus anterior.
The Medial Wall: Serratus Anterior and the Rib Cage
The medial wall of the axilla is a crucial structure, providing stability and facilitating movement of the scapula. It is primarily formed by the serratus anterior muscle and the underlying thoracic wall, specifically ribs 1 through 4, and sometimes 5. Understanding the anatomy of this wall is vital for comprehending the biomechanics of the shoulder and the potential clinical implications of injuries to this region.
Defining the Medial Boundary
The medial wall extends from the apex of the axilla, near the cervicoaxillary canal, down to the level of the fourth or fifth rib. The rib interspaces and the intercostal muscles also contribute to its structure, though the dominant feature is undoubtedly the serratus anterior. This muscle acts as a powerful link between the scapula and the rib cage, playing a critical role in protraction, upward rotation, and stabilization of the scapula against the thoracic wall.
Serratus Anterior: The Boxer’s Muscle
The serratus anterior, often referred to as the "boxer’s muscle" due to its importance in protracting the arm during punching, is a broad, flat muscle that originates from the outer surfaces and superior borders of the upper ribs.
Specifically, its digitations arise from ribs 1 through 8 or 9, depending on the individual anatomy. These digitations interdigitate with the external oblique muscle, further anchoring the muscle to the rib cage.
Origins and Insertions
The origin of the serratus anterior is along the lateral aspects of ribs 1-8/9.
From there, the muscle fibers run posteriorly and medially, wrapping around the rib cage to insert onto the anterior surface of the medial border of the scapula.
This extensive insertion ensures a strong connection between the scapula and the torso. The superior digitations attach near the superior angle, the intermediate digitations insert along the medial border, and the inferior digitations converge near the inferior angle of the scapula.
The Long Thoracic Nerve: A Vulnerable Pathway
Perhaps the most clinically significant aspect of the medial axillary wall is its relationship with the long thoracic nerve. This nerve, arising from the roots of the brachial plexus (C5, C6, and C7), courses along the surface of the serratus anterior muscle.
It is responsible for innervating the entire muscle, and injury to this nerve can have devastating consequences.
Winged Scapula and Nerve Damage
Damage to the long thoracic nerve, often resulting from trauma, surgery, or repetitive overhead movements, leads to paralysis of the serratus anterior. This paralysis manifests as a winged scapula, where the medial border of the scapula protrudes prominently from the back, especially when the arm is flexed or abducted.
The inability to properly stabilize the scapula affects a wide range of movements, significantly impacting upper limb function and causing chronic pain. Early diagnosis and management are crucial to minimize long-term disability.
The muscles of the posterior wall create a dynamic interface with the humerus and shoulder joint. Now, shifting our attention medially, we encounter the wall defined by the rib cage and a powerful muscle that secures the scapula: the serratus anterior.
The Lateral Wall: A Bony Groove
In stark contrast to the broad muscular expanses of the other axillary walls, the lateral wall presents a uniquely defined and limited structure. Its character is primarily dictated by a bony landmark of the humerus and the muscles that intimately associate with it. Understanding the lateral wall necessitates appreciating its narrow dimensions and the critical roles of the muscles that attach to it.
Defining the Lateral Boundary
The lateral wall of the axilla is essentially formed by the intertubercular groove (also known as the bicipital groove) of the humerus. This groove is a deep furrow located between the greater and lesser tubercles on the proximal end of the humerus.
It serves as a critical passageway and attachment site for muscles that act upon the shoulder joint.
Muscular Attachments: A Constrained Space
The muscles directly associated with the lateral wall, specifically the intertubercular groove, are the biceps brachii (short head) and the coracobrachialis.
The tendon of the long head of the biceps brachii passes through the intertubercular groove, although it does not directly attach to it, it’s close proximity is crucial to the regional anatomy.
The short head of the biceps brachii, along with the coracobrachialis, originates from the coracoid process of the scapula.
They then insert onto the humerus in the vicinity of the intertubercular groove. These muscles contribute to flexion and adduction of the arm, and shoulder stability.
The tight relationship of these muscles to the humerus within the axilla highlights their roles in both movement and structural integrity.
The Narrowest Dimension
The lateral wall is notable for being the narrowest of all the axillary walls. This constriction is due to the bony structure of the humerus and the limited space available for muscular attachments. The relatively confined space of the lateral wall makes it especially vulnerable to compression or injury.
Understanding the anatomy of the lateral wall is essential for diagnosing and treating conditions affecting the shoulder and upper arm. Pathologies may include rotator cuff injuries and nerve compressions.
Axillary Vasculature: Arteries and Veins
Having navigated the bony confines of the lateral wall, our journey into the axilla now turns to the critical vascular structures that traverse this region. The axillary artery and vein form the lifeline of the upper limb, providing essential blood supply and drainage. Understanding their intricate paths, branches, and clinical implications is paramount in diagnosing and managing a range of conditions.
The Axillary Artery: A Lifeline to the Arm
The axillary artery, the primary source of arterial blood for the upper limb, is a direct continuation of the subclavian artery. It officially becomes the axillary artery as it crosses the lateral border of the first rib.
Course and Divisions
The axillary artery’s course through the axilla is often described in three parts relative to the pectoralis minor muscle, a useful landmark for surgeons and clinicians:
-
First Part: Proximal to the pectoralis minor muscle, extending from the lateral border of the first rib to the superior border of the pectoralis minor.
-
Second Part: Located posterior to the pectoralis minor muscle.
-
Third Part: Distal to the pectoralis minor muscle, stretching from the inferior border of the pectoralis minor to the inferior border of the teres major, where it becomes the brachial artery.
These divisions are not merely descriptive; they serve as a crucial reference for identifying the origin points of the artery’s major branches.
Major Branches and Their Significance
The axillary artery gives rise to several vital branches, each supplying blood to various structures in the shoulder, chest, and arm:
-
Superior Thoracic Artery: Arising from the first part, it supplies the superior portion of the pectoral region.
-
Thoracoacromial Artery: Originating from the second part, this artery has four branches (pectoral, acromial, deltoid, and clavicular) that supply the shoulder and pectoral region. Its consistent presence makes it a valuable landmark during surgical procedures.
-
Lateral Thoracic Artery: Also from the second part, this artery supplies the serratus anterior muscle and the lateral aspect of the breast. It is of particular importance in breast cancer surgery, where it may be ligated.
-
Subscapular Artery: The largest branch, arising from the third part, it quickly divides into the circumflex scapular artery and the thoracodorsal artery.
The circumflex scapular artery participates in an anastomosis around the scapula.
The thoracodorsal artery supplies the latissimus dorsi muscle, making it a critical consideration during latissimus dorsi flap procedures.
-
Anterior Circumflex Humeral Artery: Arising from the third part, it runs laterally around the surgical neck of the humerus, supplying the shoulder joint and humerus.
-
Posterior Circumflex Humeral Artery: Also from the third part, this artery, along with the axillary nerve, passes through the quadrangular space. It supplies the deltoid muscle and shoulder joint. This artery is vulnerable in shoulder dislocations and humeral neck fractures.
Clinical Implications
Compromise to the axillary artery can have severe consequences for the upper limb.
-
Aneurysms: Axillary artery aneurysms, although rare, can occur due to trauma or repetitive overhead movements. They may present with pain, swelling, or even neurological symptoms due to compression of the brachial plexus.
-
Blockages: Occlusion of the axillary artery, whether due to thrombosis or embolism, can lead to acute limb ischemia, characterized by pain, pallor, pulselessness, paresthesia, and paralysis. Prompt diagnosis and intervention, often involving thrombolysis or surgical bypass, are essential to prevent irreversible damage.
-
Axillary artery injuries during surgery: This is a risk during procedures such as mastectomy or axillary lymph node dissection. Understanding the artery’s precise location and variations is crucial to avoid iatrogenic injury.
The Axillary Vein: Drainage of the Upper Limb
The axillary vein is responsible for draining blood from the upper limb and returning it to the central circulation. It begins as the basilic vein joins the brachial veins, becoming the axillary vein at the inferior border of the teres major muscle.
Course and Tributaries
The axillary vein runs medial and anterior to the axillary artery, generally following a similar course through the axilla.
Its major tributaries mirror the branches of the axillary artery, collecting blood from the corresponding regions.
These include the basilic vein, cephalic vein (which drains into the axillary vein near the clavicle), subscapular vein, lateral thoracic vein, and thoracoacromial vein.
Clinical Implications
The axillary vein is susceptible to various clinical conditions that can compromise venous return from the upper limb.
-
Thrombosis: Axillary vein thrombosis, also known as Paget-Schroetter syndrome, can occur due to repetitive arm movements or compression of the vein in the thoracic outlet. It can present with arm swelling, pain, and cyanosis. Anticoagulation and, in some cases, thrombolysis may be required.
-
Catheter Placement: The axillary vein is a common site for central venous catheter placement. However, this procedure carries risks, including thrombosis, infection, and pneumothorax. Ultrasound guidance is increasingly used to minimize these complications.
-
Venous Compression: External compression of the axillary vein, such as by a tumor or enlarged lymph nodes, can lead to upper extremity edema. Identifying and addressing the underlying cause is crucial to relieve the compression and restore venous flow.
Understanding the anatomy and clinical relevance of the axillary vasculature is critical for healthcare professionals involved in the diagnosis and management of conditions affecting the upper limb. A thorough knowledge of the axillary artery and vein, their branches, and potential pathologies allows for more effective interventions and improved patient outcomes.
The Brachial Plexus: Nerves of the Arm
Having navigated the complex network of vessels supplying the upper limb, we now turn our attention to the intricate neural network that controls its function: the brachial plexus. This complex structure, originating in the neck and traversing the axilla, is responsible for both motor and sensory innervation of the entire arm.
Understanding its organization, potential points of injury, and clinical manifestations is crucial for any clinician managing upper limb conditions.
Formation of the Brachial Plexus: Roots to Branches
The brachial plexus is formed by the ventral rami of the spinal nerves C5, C6, C7, C8, and T1. These nerve roots emerge from the intervertebral foramina and converge to form the trunks of the brachial plexus.
Roots
The roots (C5-T1) are the starting point of the brachial plexus. They emerge from the spinal cord and travel through the neck to converge and form the trunks.
Trunks
The roots then unite to form three trunks:
- The superior trunk, formed by the union of C5 and C6 roots.
- The middle trunk, which is simply a continuation of the C7 root.
- The inferior trunk, formed by the union of C8 and T1 roots.
These trunks then traverse the posterior triangle of the neck before entering the axilla.
Divisions
As each trunk passes over the first rib, it divides into an anterior and a posterior division. The anterior divisions generally supply the anterior (flexor) compartment of the upper limb, while the posterior divisions supply the posterior (extensor) compartment.
Cords
The divisions then recombine to form three cords, named according to their relationship to the axillary artery:
- The lateral cord, formed by the anterior divisions of the superior and middle trunks.
- The posterior cord, formed by all three posterior divisions.
- The medial cord, formed by the anterior division of the inferior trunk.
Branches
Finally, the cords give rise to the major terminal branches that innervate the upper limb muscles and skin. These branches include:
- The musculocutaneous nerve (from the lateral cord).
- The axillary nerve (from the posterior cord).
- The radial nerve (from the posterior cord).
- The median nerve (from both the lateral and medial cords).
- The ulnar nerve (from the medial cord).
Nerve Root Contributions to Upper Limb Nerves
Each major nerve of the upper limb receives fibers from specific nerve roots of the brachial plexus. Understanding these contributions is essential for localizing the site of injury in cases of nerve damage.
- The musculocutaneous nerve receives fibers primarily from C5, C6, and C7, and innervates the muscles of the anterior compartment of the arm (biceps brachii, brachialis, and coracobrachialis) and provides sensory innervation to the lateral forearm.
- The axillary nerve, arising from the posterior cord (C5 and C6), innervates the deltoid and teres minor muscles, as well as providing sensory innervation to the skin over the lateral aspect of the shoulder.
- The radial nerve, the largest branch of the brachial plexus (C5-T1), innervates the muscles of the posterior arm and forearm, responsible for extension at the elbow, wrist, and fingers. It also provides sensory innervation to the posterior arm, forearm, and dorsolateral hand.
- The median nerve receives fibers from C5-T1 (via both lateral and medial cords) and innervates most of the forearm flexors (except flexor carpi ulnaris) and several intrinsic hand muscles. It also provides sensory innervation to the palmar aspect of the thumb, index, middle, and radial half of the ring finger.
- The ulnar nerve originates from the medial cord (C8 and T1) and innervates the flexor carpi ulnaris and the medial half of the flexor digitorum profundus in the forearm, as well as most of the intrinsic hand muscles. It provides sensory innervation to the little finger and the medial half of the ring finger.
Clinical Implications of Brachial Plexus Injuries
Because of its complex anatomy and exposed location, the brachial plexus is vulnerable to injury. These injuries can result in significant functional deficits, depending on the severity and location of the damage.
Erb’s Palsy
Erb’s palsy, also known as waiter’s tip deformity, typically results from injury to the upper trunk of the brachial plexus (C5 and C6 roots). This can occur during a difficult delivery, particularly with shoulder dystocia, or from trauma to the neck.
The characteristic presentation involves weakness or paralysis of the shoulder and arm muscles innervated by C5 and C6, leading to adduction and internal rotation of the arm, extension of the elbow, pronation of the forearm, and flexion of the wrist (the "waiter’s tip" position).
Klumpke’s Palsy
Klumpke’s palsy results from injury to the lower trunk of the brachial plexus (C8 and T1 roots). This can also occur during childbirth if there is excessive traction on the abducted arm or from trauma such as a fall onto an outstretched arm.
The resulting deficits affect the intrinsic muscles of the hand, leading to a claw hand deformity (hyperextension of the metacarpophalangeal joints and flexion of the interphalangeal joints). There may also be sensory loss along the ulnar aspect of the forearm and hand.
In severe cases, Horner’s syndrome (ptosis, miosis, anhidrosis) may be present due to damage to the sympathetic fibers that travel with the T1 nerve root.
Lymph Nodes: Guardians of the Axilla and Gatekeepers of Metastasis
Having explored the intricate neural pathways of the brachial plexus, it’s time to shift our focus to another vital component of the axilla: the lymphatic system. This network of vessels and nodes acts as both a drainage system and a crucial part of the immune system, playing a pivotal role in detecting and combating infection and disease.
Within the axilla, the lymph nodes are strategically positioned to monitor and filter lymph fluid collected from the upper limb, thorax, and breast. Their involvement in metastasis, particularly in the context of breast cancer, makes their understanding paramount for clinicians.
Location and Arrangement of Axillary Lymph Nodes
The axillary lymph nodes, numbering between 20 and 40, are embedded in the adipose tissue within the axilla. They are organized into several groups, each with a specific location and drainage territory. Understanding their arrangement is critical for surgical planning and accurate interpretation of imaging studies.
The main groups of axillary lymph nodes are:
-
Pectoral (Anterior) Nodes: Located along the lower border of the pectoralis minor muscle, these nodes receive lymph primarily from the anterior thoracic wall, including the breast.
-
Lateral Nodes: Situated along the axillary vein, these nodes drain the majority of lymph from the upper limb.
-
Subscapular (Posterior) Nodes: Found along the subscapular artery, these nodes receive lymph from the posterior aspect of the thoracic wall and the scapular region.
-
Central Nodes: Located deep within the axilla, these nodes receive lymph from the pectoral, lateral, and subscapular nodes.
-
Apical Nodes: Situated at the apex of the axilla, near the clavicle, these nodes receive lymph from all other axillary groups. The efferent vessels from the apical nodes then drain into the subclavian lymphatic trunk.
Drainage Patterns of the Axillary Lymph Nodes
The axillary lymph nodes don’t operate in isolation. They’re interconnected, forming a hierarchical drainage pathway. Understanding this pathway is essential for predicting the spread of cancer and guiding surgical interventions like sentinel lymph node biopsy.
Lymph from the upper limb generally flows first to the lateral nodes, before proceeding to the central nodes. Lymph from the breast primarily drains into the pectoral nodes, which also then drain into the central nodes. From the central nodes, lymph ascends to the apical nodes, the final common pathway within the axilla.
From the apical nodes, lymph continues its journey via the subclavian lymphatic trunk, eventually emptying into the venous system. This connection to the systemic circulation is what allows for distant metastasis if cancer cells manage to bypass the lymphatic filters.
Clinical Significance: Metastasis, Breast Cancer, and Lymphadenopathy
The axillary lymph nodes are often the first site of metastasis for breast cancer. Cancer cells from the breast can travel through the lymphatic vessels and become trapped in the nodes, where they can begin to grow and form secondary tumors.
The involvement of axillary lymph nodes is a crucial factor in determining the stage of breast cancer and guiding treatment decisions. The more nodes involved, the more advanced the cancer is considered to be, and the more aggressive the treatment approach may need to be.
Sentinel lymph node biopsy (SLNB) is a surgical procedure used to identify the first lymph node(s) to which cancer cells are most likely to spread from a primary tumor. This technique helps surgeons determine whether the cancer has spread to the axillary lymph nodes without removing all of them, reducing the risk of lymphedema.
Axillary lymphadenopathy, or enlarged lymph nodes in the axilla, can be a sign of infection, inflammation, or malignancy. While breast cancer is a major concern, other causes of lymphadenopathy include infections of the upper limb, lymphoma, and other types of cancer.
Palpable or suspicious lymph nodes warrant further investigation, typically involving imaging studies such as ultrasound or CT scan, and possibly a biopsy to determine the cause of the enlargement. Careful evaluation is essential for timely diagnosis and appropriate management.
In conclusion, the axillary lymph nodes are more than just anatomical structures. They are active participants in immune surveillance and critical indicators of disease, especially in the context of breast cancer. A thorough understanding of their location, drainage patterns, and clinical significance is indispensable for healthcare professionals involved in the diagnosis and treatment of upper limb and breast conditions.
Clinical Significance: Axillary Pathologies
The axilla, as a crucial anatomical crossroads, is susceptible to a variety of pathological conditions. Understanding these conditions is paramount for effective diagnosis, treatment, and overall patient care. The pathologies affecting this region range from inflammatory processes and metastatic disease to traumatic injuries and complications arising from surgical interventions. Let’s delve into some of the most clinically relevant aspects of axillary pathologies.
Axillary Lymphadenopathy
Axillary lymphadenopathy, or the enlargement of axillary lymph nodes, is a common clinical finding. It signals an underlying pathological process that warrants careful investigation. While often benign and self-limiting, lymphadenopathy can also indicate serious underlying conditions.
Causes of Axillary Lymphadenopathy
The causes of axillary lymphadenopathy are diverse, spanning infectious, inflammatory, and neoplastic etiologies. Infections, both local and systemic, are frequent culprits. Examples include bacterial infections like cellulitis, viral infections such as mononucleosis, and less common infections like cat-scratch disease.
Malignancies represent another significant category. Lymphoma, both Hodgkin’s and non-Hodgkin’s, can manifest as axillary lymph node enlargement. Metastatic disease, particularly from breast cancer, is a major concern and often the primary reason for clinical evaluation of the axilla.
Inflammatory conditions, such as rheumatoid arthritis and sarcoidosis, can also lead to lymph node enlargement. Other less common causes include reactions to medications and certain autoimmune disorders.
Diagnosis and Management
The diagnostic approach to axillary lymphadenopathy begins with a thorough history and physical examination. Factors such as the size, consistency, and location of the enlarged nodes are noted. The presence of other symptoms, such as fever, weight loss, or night sweats, can provide further clues.
Imaging studies, including ultrasound, CT scans, or MRI, are often employed to further evaluate the lymph nodes. Ultrasound-guided fine-needle aspiration (FNA) or core biopsy is frequently performed to obtain tissue for pathological examination.
Management strategies depend on the underlying cause. Infections typically require antibiotic or antiviral therapy. Inflammatory conditions may necessitate immunosuppressant medications. Malignancies often require a combination of surgery, radiation therapy, and chemotherapy. Regular follow-up is crucial to monitor treatment response and detect any recurrence.
Breast Cancer Metastasis
The axilla is a primary site for the regional spread of breast cancer. Axillary lymph node involvement is a significant prognostic factor and a key determinant in treatment planning.
Spread to Axillary Lymph Nodes
Breast cancer cells can spread to the axillary lymph nodes through lymphatic vessels. The sentinel lymph node, the first lymph node to receive drainage from the primary tumor, is often the initial site of metastasis. From there, cancer cells can spread to other axillary lymph nodes and potentially to distant sites.
Staging and Treatment Implications
The presence and extent of axillary lymph node involvement are crucial for staging breast cancer. The number of involved lymph nodes directly impacts the stage of the disease and influences treatment decisions.
Axillary lymph node dissection (ALND), the surgical removal of axillary lymph nodes, was historically a standard component of breast cancer treatment. However, sentinel lymph node biopsy (SLNB) has largely replaced ALND in early-stage breast cancer with clinically negative axilla, reducing the risk of lymphedema and other complications.
Systemic therapies, including chemotherapy, hormone therapy, and targeted therapies, are often administered to eradicate any remaining cancer cells and reduce the risk of recurrence. Radiation therapy to the axilla may also be considered in certain cases.
Injuries and Trauma
The axilla, with its rich neurovascular content, is vulnerable to injuries resulting from trauma. Fractures of the clavicle, scapula, or humerus can indirectly impact axillary structures.
Impact of Fractures on Axillary Structures
Clavicle fractures, particularly those involving the middle third, can potentially injure the subclavian vessels and the brachial plexus. Scapular fractures, while less common, can affect the subscapular artery and nerve. Humeral fractures, especially those involving the proximal humerus, can compromise the axillary artery and nerve.
Penetrating injuries, such as stab wounds or gunshot wounds, can directly damage axillary vessels and nerves. Blunt trauma can cause contusions, hematomas, and even compartment syndrome within the axilla.
Prompt diagnosis and management are essential to minimize long-term complications. Vascular injuries may require surgical repair or endovascular intervention. Nerve injuries may necessitate surgical exploration and repair or reconstruction. Physical therapy and rehabilitation are crucial for restoring function.
Surgical Considerations
The axilla is a frequent target for surgical interventions, both for diagnostic and therapeutic purposes. Understanding the anatomy of the axilla is crucial for minimizing complications.
Approaches to the Axilla
Surgical approaches to the axilla vary depending on the specific indication. Axillary dissection, sentinel lymph node biopsy, and procedures to address vascular or nerve injuries require meticulous surgical technique.
Nerve Blocks
Regional anesthesia techniques, such as axillary nerve blocks, are commonly used for upper limb surgeries. These blocks provide excellent pain control and reduce the need for general anesthesia.
Surgical Complications
Surgical procedures in the axilla carry the risk of complications, including lymphedema, seroma formation, wound infection, and nerve injury. Lymphedema, the chronic swelling of the arm due to impaired lymphatic drainage, is a particularly debilitating complication.
Meticulous surgical technique, careful patient selection, and appropriate postoperative management are essential to minimize the risk of surgical complications. Postoperative physical therapy and lymphedema management strategies can help to improve outcomes and quality of life.
Functional Role: Movement and Stability
Beyond its intricate anatomy and susceptibility to pathologies, the axilla plays a crucial functional role in enabling upper limb movement, ensuring adequate circulation and nerve supply, and providing a protective conduit for vital structures. Understanding these functional aspects adds another layer of appreciation for the complexity and importance of this anatomical region.
Movement and Upper Limb Function
The axilla, by virtue of the muscles that form its walls, is intrinsically linked to the dynamic capabilities of the upper limb. These muscles, including the pectoralis major, latissimus dorsi, subscapularis, teres major, and serratus anterior, contribute to a wide range of movements at the shoulder joint.
These actions range from powerful adduction, internal rotation, and extension to essential protraction and stabilization of the scapula. The coordinated action of these muscles, many of which have attachments directly within or bordering the axilla, is fundamental to tasks such as lifting, pushing, pulling, and reaching. Any compromise to these muscles or their associated nerve supply can profoundly impact upper limb function and overall quality of life.
Furthermore, the axilla’s role as a passageway allows the upper limb to articulate effectively with the torso. It permits a range of motion that would otherwise be constrained, as the muscles and tendons need a space to move. The axilla offers this space.
Circulation and Nerve Supply to the Arm
The axilla serves as the primary conduit for the major neurovascular structures supplying the upper limb. The axillary artery and vein, along with the brachial plexus, traverse this region, ensuring the arm receives adequate blood flow and nerve innervation.
The Axillary Artery and Vein
The axillary artery, a direct continuation of the subclavian artery, is the lifeline of the upper limb. Its branches supply oxygenated blood to the muscles, bones, and skin of the shoulder, arm, and hand. Blockage or injury to the axillary artery can have devastating consequences, leading to ischemia, tissue damage, and potentially limb loss.
Similarly, the axillary vein provides venous drainage, returning deoxygenated blood from the upper limb to the central circulation. Thrombosis or compression of the axillary vein can result in swelling, pain, and impaired limb function.
The Brachial Plexus
The brachial plexus, a complex network of nerves originating from the spinal cord, innervates nearly all the muscles and skin of the upper limb. This intricate network, formed by the ventral rami of spinal nerves C5-T1, passes through the axilla, giving rise to major peripheral nerves such as the musculocutaneous, axillary, radial, median, and ulnar nerves.
Damage to the brachial plexus, whether from trauma, compression, or inflammation, can result in a wide range of neurological deficits, including weakness, paralysis, sensory loss, and chronic pain. Conditions like Erb’s palsy and Klumpke’s palsy, often seen in newborns after difficult deliveries, are classic examples of brachial plexus injuries with significant functional implications.
Stability and Protection of Vital Structures
The walls of the axilla, composed of muscles, fascia, and bone, play a critical role in providing both stability and protection to the vital neurovascular structures within. These walls form a protective cage, shielding the axillary artery, vein, brachial plexus, and lymph nodes from external trauma and compression.
The muscular walls of the axilla help to maintain the anatomical integrity of the region, preventing excessive movement or displacement of the neurovascular structures during shoulder and arm movements. This is particularly important during strenuous activities or in cases of trauma, where the axilla is vulnerable to injury.
Furthermore, the axillary lymph nodes, strategically located within the axilla, play a crucial role in immune surveillance and defense. They filter lymph fluid, removing bacteria, viruses, and other pathogens, and serve as a staging ground for immune cells.
The walls of the axilla thus serve as a line of defense, containing and preventing the spread of infection or malignancy. Their location within the axilla also makes them a critical site for monitoring disease progression, as evidenced by their involvement in breast cancer metastasis.
In conclusion, the axilla is far more than just an anatomical space. It is a dynamic region that enables upper limb movement, ensures adequate circulation and nerve supply, and provides essential stability and protection to vital structures. A thorough understanding of these functional roles is paramount for clinicians in diagnosing and managing a wide range of conditions affecting the upper limb and the axilla itself.
Walls of Axilla: Frequently Asked Questions
[The Axilla, commonly known as the armpit, is a pyramidal space between the arm and the chest. Understanding its walls and contents is critical in clinical practice. Here are some frequently asked questions to clarify key concepts.]
What are the boundaries of the axilla walls?
The axilla has four walls: anterior, posterior, medial, and lateral. The anterior wall is formed by the pectoralis major and minor muscles. The posterior wall consists of the subscapularis, teres major, and latissimus dorsi muscles. The medial wall is made up of the serratus anterior muscle and the thoracic wall. Lastly, the lateral wall is the intertubercular groove of the humerus.
What structures pass through the axilla?
Numerous important structures traverse the axilla, including the axillary artery and vein, branches of the brachial plexus, and lymph nodes. These vessels and nerves supply the upper limb. Understanding their course relative to the walls of the axilla is crucial for surgical procedures and diagnosing injuries in the region.
What is the clinical significance of axillary lymph nodes?
The axillary lymph nodes are vital for lymphatic drainage of the upper limb and breast. They are often involved in the spread of breast cancer. Enlarged or tender axillary lymph nodes can indicate infection, inflammation, or malignancy. Therefore, palpation of the walls of axilla is an important part of clinical examination.
How can damage to the walls of the axilla impact function?
Injuries affecting the walls of the axilla, such as those involving the muscles or the brachial plexus, can lead to significant functional deficits. This can include weakness or paralysis of the upper limb, sensory loss, and circulatory problems. Depending on the affected wall, these deficits can manifest in different patterns.
Alright, that pretty much covers the walls of axilla! Hopefully, this has shed some light on this important anatomical region. Keep that knowledge handy, and you’ll be well-equipped to tackle any clinical scenarios involving the walls of axilla. Until next time!