Understanding the heart’s intricate mechanisms is crucial in cardiology. The visceral pericardium, a serous membrane, directly envelopes the myocardium. Research from institutions like the National Institutes of Health continues to reveal its significant role. This membrane is not just a protective layer; the visceral pericardium function actively contributes to cardiac efficiency. Furthermore, advancements in imaging technologies, such as echocardiography, allow clinicians and researchers to better assess the functional dynamics of this critical structure. Alterations in visceral pericardium function can significantly impact overall cardiovascular health and might be evaluated by expert like Dr. Emily Carter for further examination, impacting blood supply and heart rate.
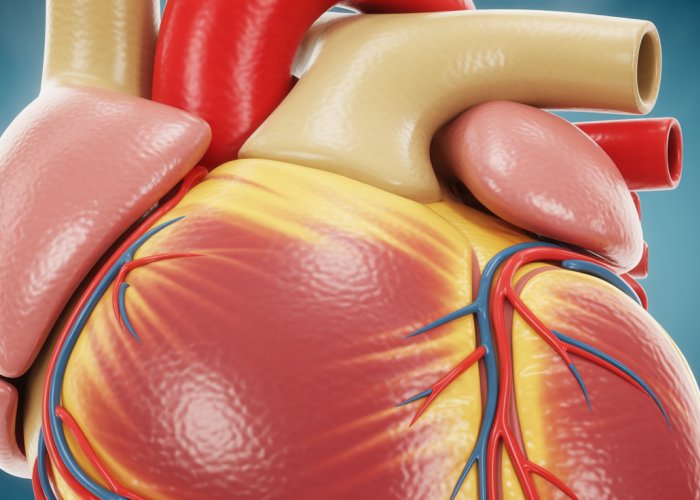
The human heart, a tireless engine, orchestrates the circulatory system’s intricate dance, delivering life-sustaining oxygen and nutrients throughout the body. Its continuous operation demands robust protection, which is provided by a multi-layered sac known as the pericardium.
The Heart: Central to Circulation
The heart is more than just a pump; it’s the central command center of the circulatory system. Its rhythmic contractions propel blood through a vast network of vessels, ensuring every cell receives the resources it needs to function. Any disruption to this vital organ can have profound consequences for overall health.
The Pericardium: A Protective Shield
Encasing the heart is the pericardium, a double-layered structure that acts as a protective shield. This sac safeguards the heart from external trauma, reduces friction during its ceaseless activity, and helps prevent over-dilation.
The pericardium comprises two primary layers: the fibrous pericardium (outer layer) and the serous pericardium (inner layer). The serous pericardium is further divided into two layers: the parietal pericardium, which lines the fibrous pericardium, and the visceral pericardium, also known as the epicardium, which directly adheres to the heart’s surface.
The Visceral Pericardium (Epicardium): A Closer Look
The visceral pericardium, or epicardium, is the outermost layer of the heart wall itself. It’s a thin, serous membrane composed of a single layer of mesothelial cells overlying a layer of connective tissue.
This intimate association with the myocardium, the heart’s muscular layer, positions the epicardium to play a crucial role in cardiac function, including tissue repair and inflammation regulation.
The significance of the visceral pericardium extends beyond simple protection. It actively participates in maintaining cardiac homeostasis. Understanding its structure, function, and relationship with other pericardial layers is paramount to comprehending cardiovascular health and disease.
Thesis Statement
The Visceral Pericardium, also known as the Epicardium, plays a vital role in Cardiac Function, and understanding its structure and relationship with other pericardial layers is crucial for comprehending cardiovascular health and disease.
The significance of the pericardium in protecting the heart and facilitating its function cannot be overstated. But to truly appreciate its role, a closer examination of its individual components is essential, beginning with the visceral pericardium, or epicardium.
Anatomy and Microstructure: Exploring the Visceral Pericardium
This section delves into the intricate anatomy of the visceral pericardium, exploring its cellular composition, histological features, and spatial relationship with adjacent structures. Understanding these details is critical to appreciating the epicardium’s role in cardiac health and disease.
Histology and Cellular Composition
The visceral pericardium, or epicardium, is not simply a passive covering; it’s a dynamic tissue with a complex microstructure. This outermost layer of the heart wall is primarily composed of a single layer of flattened mesothelial cells that rest on a thin layer of connective tissue.
Beneath the mesothelial layer lies a sub-epicardial space containing fibroblasts, adipocytes, nerve fibers, and blood vessels, all embedded in a collagen-rich matrix.
Mesothelial cells are key players, responsible for producing lubricating pericardial fluid and mediating inflammatory responses.
Fibroblasts contribute to the structural integrity of the epicardium by synthesizing collagen and other extracellular matrix components.
Relationship to Other Pericardial Layers
The visceral pericardium is intimately connected to the other layers of the pericardium, forming a cohesive protective unit. It’s essential to understand these relationships to appreciate the overall function of the pericardial sac.
Serous Pericardium
The serous pericardium is a double-layered membrane. The visceral pericardium (epicardium) is one layer, and the other is the parietal pericardium, which lines the inner surface of the fibrous pericardium.
The parietal and visceral layers are continuous, folding back on themselves at the base of the heart. This creates a closed sac surrounding the heart.
Fibrous Pericardium
The fibrous pericardium is the outermost layer. It’s a tough, inelastic sac that provides structural support and protection.
It is not directly attached to the heart. The parietal pericardium lines the inner surface of the fibrous pericardium, and the visceral pericardium covers the heart’s surface.
The Pericardial Cavity and Fluid
Between the visceral and parietal layers of the serous pericardium lies the pericardial cavity.
This potential space normally contains a small amount (15-50 ml) of pericardial fluid, an ultrafiltrate of plasma secreted by the mesothelial cells.
The pericardial fluid acts as a lubricant, reducing friction between the beating heart and the surrounding structures.
This lubrication is crucial for efficient cardiac function. It enables the heart to move freely within the pericardial sac.
Proximity to the Myocardium: A Critical Interface
The visceral pericardium’s close proximity to the myocardium, the heart’s muscular layer, is critical to its role in cardiac function.
This intimate association facilitates cell-cell interactions and paracrine signaling, influencing myocardial growth, repair, and inflammation.
The epicardium can release various growth factors and cytokines that affect myocardial cells. These factors can promote angiogenesis, fibrosis, and other processes.
Emerging evidence suggests that the epicardium plays a crucial role in cardiac regeneration following injury.
Functions: How the Visceral Pericardium Supports a Healthy Heart
The visceral pericardium, far from being a mere encasement, actively contributes to the heart’s well-being. Its functions extend beyond simple physical containment, playing a crucial role in protecting, lubricating, and modulating cardiac volume. These multifaceted contributions are integral to maintaining overall cardiovascular health and ensuring efficient cardiac function.
Protection and Structural Integrity
The pericardium, with the epicardium as its visceral layer, acts as a physical barrier safeguarding the heart from external trauma and infectious agents. This protective function is paramount, particularly given the heart’s constant motion and vulnerability within the chest cavity.
The epicardium’s connective tissue provides a structural framework, offering support and maintaining the heart’s shape. It limits excessive movement, preventing displacement during periods of high activity or stress.
Lubrication: Minimizing Friction
A critical function of the visceral pericardium, in conjunction with the parietal pericardium, is the production and maintenance of pericardial fluid within the pericardial cavity. This fluid acts as a natural lubricant, significantly reducing friction between the heart and surrounding structures during the continuous cardiac cycle.
The mesothelial cells of the visceral pericardium are responsible for secreting this lubricating fluid. This ensures smooth, unhindered heartbeats. Any disruption to this lubrication, such as in pericarditis, can lead to painful friction rubs and impaired cardiac function.
Volume Regulation: Preventing Over-Dilation
The pericardium’s inherent elasticity plays a vital role in preventing acute over-dilation of the heart. While it allows for normal physiological expansion during increased blood volume, it restricts excessive stretching that could compromise cardiac muscle integrity.
This volume-regulating function is particularly important in conditions where the heart is at risk of overfilling, such as in cases of rapid fluid administration or certain types of heart failure. The pericardium acts as a natural constraint, preventing the heart from exceeding its optimal functional volume.
Contribution to Cardiovascular Health
In essence, the visceral pericardium’s diverse functions converge to support overall cardiovascular health. Its protective barrier, lubricating action, and volume-regulating properties contribute synergistically to efficient cardiac function. By minimizing friction, preventing over-dilation, and shielding the heart from external threats, the visceral pericardium ensures the heart can perform its vital pumping function optimally. This maintains the circulatory system’s integrity.
Compromise in any of these functions, due to inflammation, infection, or other pathological processes, can lead to significant cardiovascular complications, underscoring the visceral pericardium’s importance in cardiac physiology.
Clinical Relevance: Pericardial Diseases and Their Impact
Having explored the anatomy and vital functions of the visceral pericardium, it’s crucial to understand how diseases affecting this structure can compromise cardiac health. Pericardial diseases, while sometimes overlooked, can have significant, even life-threatening, consequences for cardiac function.
Pericarditis: Inflammation’s Cascade
Pericarditis, an inflammation of the pericardium, represents a spectrum of clinical presentations.
Causes and Triggers
The etiology of pericarditis is diverse, ranging from infectious agents to systemic inflammatory conditions. Viral infections are the most common cause, but bacterial, fungal, and parasitic infections can also trigger the condition.
Autoimmune diseases like lupus, rheumatoid arthritis, and scleroderma are frequently associated with pericarditis. Trauma, either blunt or penetrating, and certain medications can also lead to pericardial inflammation. In some instances, the cause remains elusive, termed idiopathic pericarditis.
Symptomatic Presentation and Diagnosis
Patients with pericarditis typically present with sharp, stabbing chest pain, often exacerbated by breathing or lying down. Fever, shortness of breath, and fatigue can also accompany the chest pain.
Diagnosis involves a combination of clinical assessment, electrocardiography (ECG), and echocardiography. ECG changes, such as widespread ST-segment elevation, are characteristic of pericarditis. Echocardiography helps to identify pericardial effusion, a common complication of pericarditis.
Impact on Visceral Pericardium and Cardiac Function
Inflammation of the visceral pericardium can lead to several detrimental effects. The inflammatory process can disrupt the delicate balance of pericardial fluid, leading to either excessive fluid accumulation (effusion) or thickening and scarring of the pericardium.
The proximity of the visceral pericardium to the myocardium means that inflammation can spread to the heart muscle itself (myocarditis or myopericarditis). This can impair cardiac contractility and lead to arrhythmias. Chronic inflammation can result in constrictive pericarditis, a condition where the thickened, scarred pericardium restricts cardiac filling.
Cardiac Tamponade: A Life-Threatening Compression
Cardiac tamponade is a critical condition characterized by compression of the heart due to fluid accumulation in the pericardial space.
Mechanism and Etiology
The pericardial space, normally containing a small amount of lubricating fluid, can rapidly fill with fluid due to pericarditis, trauma, or malignancy. This fluid accumulation increases pressure within the pericardial sac, impeding cardiac filling.
As the pressure rises, the heart chambers are compressed, reducing cardiac output. Trauma, leading to hemopericardium (blood in the pericardial sac), and malignancy, causing pericardial effusion, are other significant causes.
Hemodynamic Consequences
The hallmark of cardiac tamponade is reduced cardiac output. The compressed heart chambers cannot fill adequately during diastole, leading to a decrease in stroke volume. This, in turn, results in hypotension and shock.
Cardiac tamponade is a life-threatening emergency requiring immediate intervention.
Constrictive Pericarditis: A Restrictive Embrace
Constrictive pericarditis is a chronic condition where the pericardium becomes thickened, scarred, and rigid.
This constricts the heart, impairing its ability to expand and fill properly.
Pathophysiology and Impact on Cardiac Function
The most common cause is previous pericarditis, although surgery or radiation can also be causes. The fibrotic, inelastic pericardium restricts cardiac filling, leading to elevated systemic venous pressure and reduced cardiac output.
Clinical Manifestations
Patients with constrictive pericarditis often present with symptoms of heart failure, such as fatigue, shortness of breath, and edema. The diagnosis can be challenging, requiring a combination of clinical findings, echocardiography, and cardiac catheterization.
In conclusion, pericardial diseases, encompassing pericarditis, cardiac tamponade, and constrictive pericarditis, pose significant threats to cardiac function. A thorough understanding of their causes, symptoms, and hemodynamic consequences is essential for timely diagnosis and effective management.
Clinical manifestations of pericardial diseases, like pericarditis and cardiac tamponade, can significantly impair cardiac function. Consequently, accurate and timely diagnosis is paramount. This section delves into the diagnostic tools and imaging techniques used to assess the visceral pericardium in clinical practice. These methods help clinicians visualize the pericardium, evaluate its condition, and understand the impact of pericardial diseases on the heart.
Diagnosis and Imaging: Assessing the Visceral Pericardium in Clinical Practice
Diagnostic Approaches to Visceral Pericardium Assessment
The diagnosis of visceral pericardial involvement in cardiac diseases relies on a multi-faceted approach. It incorporates clinical evaluation, non-invasive imaging, and electrophysiological assessments.
The diagnostic process often begins with a thorough medical history and physical examination. Clinicians look for symptoms such as chest pain, dyspnea, and signs of fluid retention, which may indicate pericardial disease.
Physical Examination and Auscultation
Auscultation, listening to the heart sounds with a stethoscope, can reveal characteristic pericardial friction rubs, a hallmark of pericarditis. However, the absence of a rub does not rule out pericardial disease.
Imaging Modalities for Visualizing the Visceral Pericardium
Imaging techniques play a crucial role in visualizing the visceral pericardium and detecting abnormalities such as pericardial effusion, thickening, or inflammation. Several modalities are available, each with its strengths and limitations.
Echocardiography: A Primary Imaging Tool
Echocardiography is often the first-line imaging modality for evaluating the pericardium. It uses sound waves to create real-time images of the heart and surrounding structures, including the pericardium.
Transthoracic echocardiography (TTE), performed by placing a transducer on the chest, is the most common type. It allows for visualization of pericardial effusion, assessment of cardiac chamber size and function, and detection of signs of cardiac tamponade, such as right atrial or ventricular collapse.
Transesophageal echocardiography (TEE), which involves inserting a probe into the esophagus, provides higher-resolution images of the pericardium. It is particularly useful for evaluating patients with technically limited TTE images or for detecting subtle pericardial abnormalities.
Magnetic Resonance Imaging (MRI): Detailed Tissue Characterization
Cardiac MRI offers superior anatomical detail and tissue characterization compared to echocardiography. It can visualize the pericardium with high resolution, allowing for the detection of pericardial thickening, inflammation, and masses.
MRI is particularly useful in differentiating between constrictive pericarditis and restrictive cardiomyopathy. Two conditions that can present with similar clinical symptoms. MRI can also quantify pericardial effusion and assess for the presence of adhesions or calcifications.
Chest X-Ray: Assessing Cardiac Size and Effusion
A chest X-ray is a readily available and inexpensive imaging modality that can provide valuable information about the heart and pericardium. While it does not directly visualize the pericardium, it can detect cardiomegaly (enlarged heart) and large pericardial effusions.
However, chest X-rays have limited sensitivity for detecting small pericardial effusions or subtle pericardial abnormalities.
Electrocardiography (ECG): Assessing Cardiac Function in Pericardial Diseases
The electrocardiogram (ECG) is a non-invasive test that records the electrical activity of the heart. It plays a vital role in the diagnosis and management of pericardial diseases.
ECG Findings in Pericarditis
In acute pericarditis, the ECG typically shows widespread ST-segment elevation and PR-segment depression. These changes reflect inflammation of the myocardium adjacent to the visceral pericardium. As pericarditis resolves, the ECG may show T-wave inversions.
ECG Findings in Cardiac Tamponade
In cardiac tamponade, the ECG may show electrical alternans, a beat-to-beat variation in the amplitude of the QRS complexes. This finding reflects the swinging motion of the heart within the pericardial effusion.
The ECG can also help rule out other conditions that may mimic pericardial diseases, such as myocardial infarction.
In summary, the assessment of the visceral pericardium relies on a combination of clinical evaluation, imaging techniques, and electrophysiological assessments. Echocardiography remains the primary imaging modality, while MRI offers superior anatomical detail and tissue characterization. The ECG plays a crucial role in assessing cardiac function and detecting electrical abnormalities associated with pericardial diseases. Using these diagnostic tools effectively enables clinicians to accurately diagnose and manage conditions affecting the visceral pericardium, ultimately improving patient outcomes.
Clinical manifestations of pericardial diseases, like pericarditis and cardiac tamponade, can significantly impair cardiac function. Consequently, accurate and timely diagnosis is paramount. This section delves into the diagnostic tools and imaging techniques used to assess the visceral pericardium in clinical practice. These methods help clinicians visualize the pericardium, evaluate its condition, and understand the impact of pericardial diseases on the heart.
Future Directions and Research: Unveiling New Insights into the Visceral Pericardium
While significant strides have been made in understanding the visceral pericardium, many questions remain unanswered. Ongoing research continues to probe its complex functions and explore novel therapeutic avenues. This section will explore the cutting edge of research, focusing on emerging therapeutic targets and the exciting possibility of harnessing the epicardium for cardiac regeneration.
Unraveling the Epicardium’s Role in Cardiac Function
Current research is increasingly focused on delineating the precise mechanisms by which the visceral pericardium, or epicardium, influences cardiac function.
This includes investigating the complex interplay between the epicardium and the underlying myocardium.
Scientists are exploring the role of epicardial-derived factors (EPDCs) in regulating myocardial development, angiogenesis, and fibrosis.
Understanding these signaling pathways is critical for identifying potential targets for therapeutic intervention in various cardiac diseases.
Emerging Therapeutic Targets for Pericardial Diseases
Traditional treatments for pericardial diseases primarily focus on alleviating symptoms and reducing inflammation. However, new research is paving the way for more targeted therapies.
Anti-inflammatory Agents
Novel anti-inflammatory agents with fewer side effects are under investigation.
These aim to selectively dampen the inflammatory response in the pericardium without compromising the body’s immune system.
Immunomodulatory Therapies
For autoimmune-related pericarditis, immunomodulatory therapies are showing promise in controlling the aberrant immune response.
This involves using specific antibodies or small molecules to target immune cells involved in pericardial inflammation.
Targeting Fibrosis
In cases of constrictive pericarditis, where fibrosis is the main issue, research is focusing on developing anti-fibrotic drugs.
These drugs aim to prevent or reverse the excessive collagen deposition in the pericardium.
The Epicardium and Cardiac Regeneration
One of the most exciting areas of research is the potential of the epicardium to contribute to cardiac regeneration after injury.
Epicardial Activation
Following myocardial infarction, the epicardium undergoes activation and can give rise to progenitor cells.
These cells have the potential to differentiate into cardiomyocytes and other cardiac cell types.
Stimulating Regeneration
Researchers are exploring ways to stimulate this regenerative potential of the epicardium.
This includes using growth factors, gene therapy, and biomaterials to promote epicardial cell proliferation and differentiation.
Overcoming Challenges
However, there are also challenges.
The regenerative capacity of the epicardium is limited, and the mechanisms regulating its differentiation are not fully understood.
Further research is needed to overcome these hurdles and unlock the full potential of the epicardium for cardiac repair.
The future of pericardial research is bright, with ongoing investigations promising to unveil new insights into the epicardium’s role in cardiac health and disease. By identifying novel therapeutic targets and harnessing the regenerative potential of the epicardium, we can pave the way for more effective treatments and improved outcomes for patients with pericardial conditions.
Visceral Pericardium: FAQs
Hopefully these questions shed some further light on the visceral pericardium and its role in heart health.
What exactly is the visceral pericardium?
The visceral pericardium, also known as the epicardium, is the inner layer of the pericardium that directly covers the heart. It’s a serous membrane composed of mesothelial cells and underlying connective tissue. It plays a critical role in protecting the heart.
How does the visceral pericardium function differ from the parietal pericardium?
The parietal pericardium is the outer layer of the pericardium. The visceral pericardium function involves directly covering the heart muscle, while the parietal pericardium forms a sac around the heart, separated by the pericardial cavity.
Why is the visceral pericardium important for heart function?
The visceral pericardium function is vital because it secretes serous fluid which lubricates the heart, reducing friction as it beats. It also contains blood vessels and nerves that supply the heart muscle itself. Therefore, it protects and nurtures the heart.
Can problems with the visceral pericardium lead to heart issues?
Yes, inflammation or disease affecting the visceral pericardium can lead to conditions like pericarditis. This can impair visceral pericardium function, resulting in chest pain, fluid accumulation, and potentially even constrictive pericarditis, which restricts heart movement.
So, hopefully, this gave you a clearer picture of what’s going on with the visceral pericardium and its crucial function. Keep exploring, and remember that a healthy heart is a happy heart!