Understanding the ventral cavity subdivisions is fundamental for anyone studying human anatomy. Anatomical science, a core discipline in understanding the body, relies heavily on knowledge of these compartments. Specifically, the thoracic cavity and the abdominopelvic cavity, two major subdivisions, are crucial for housing vital organs. Moreover, the study of ventral cavity subdivisions often involves the use of medical imaging techniques to visualize and diagnose conditions within these areas. This detailed exploration of the ventral cavity subdivisions will provide a solid foundation for further studies in related medical fields.
The human body, a marvel of biological engineering, relies on intricate internal organization to maintain life. Among the most crucial aspects of this organization is the presence of body cavities – spaces within the body that house and protect our vital organs. The ventral cavity, also known as the anterior body cavity, is one such significant space.
It’s a large internal compartment situated towards the front (anterior) of the body. It’s distinguished from the dorsal (posterior) cavity which contains the brain and spinal cord. Understanding the ventral cavity is paramount to grasping how our bodies function and how disease processes can affect us.
Defining the Ventral Cavity and its Protective Role
The ventral cavity is the larger of the two major body cavities. It’s positioned towards the front of the torso. This cavity is not a single, empty space, but rather a series of interconnected spaces.
Its primary function is to provide a safe and supportive environment for the body’s essential organs. These organs include the heart, lungs, stomach, intestines, and reproductive organs. The bony structures of the rib cage and pelvis, along with surrounding muscles and connective tissues, offer a physical barrier against external trauma.
Beyond physical protection, the ventral cavity also regulates internal conditions. It helps maintain proper temperature and fluid balance. Serous membranes, which we’ll discuss later, line the cavity walls and organ surfaces, further reducing friction and preventing inflammation.
The Importance of Subdividing the Ventral Cavity
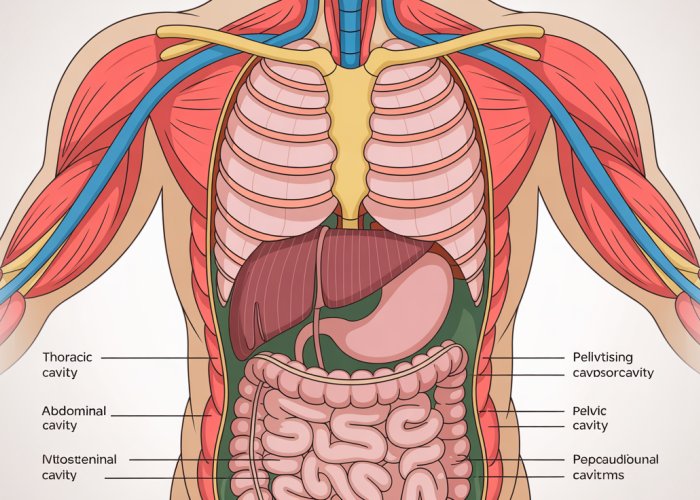
While it’s one large continuous space, the ventral cavity is subdivided into distinct regions. These include the thoracic cavity (chest), the abdominal cavity, and the pelvic cavity.
This subdivision is not arbitrary. It reflects the arrangement and functional groupings of the organs within. It also facilitates more effective study and understanding. By dividing the ventral cavity into smaller, more manageable regions, we can more easily:
-
Localize organs and structures: Knowing the boundaries of each cavity helps pinpoint the location of specific organs, which is crucial in diagnosis and treatment.
-
Understand anatomical relationships: Subdivision clarifies the spatial relationships between organs, enabling better understanding of how they interact and influence each other.
-
Compartmentalize pathology: Infections or other diseases are often limited to a specific cavity or sub-cavity. Understanding these boundaries aids in diagnosing and treating disease processes.
-
Enhance teaching and learning: Subdividing complex anatomical regions into digestible parts makes it easier for students to learn and healthcare professionals to refresh their knowledge.
Relevance for Diverse Audiences
The study of the ventral cavity is relevant to a broad spectrum of individuals.
-
Students of anatomy and physiology: An understanding of the ventral cavity is foundational for learning about the human body and its functions. It forms the basis for understanding more complex physiological processes.
-
Healthcare professionals: Physicians, nurses, and allied health professionals rely on their knowledge of the ventral cavity for accurate diagnosis, treatment planning, and surgical procedures. Knowledge of this region is critical for understanding disease processes and how they manifest.
-
Fitness and wellness professionals: Understanding the location of organs and structures within the ventral cavity can inform exercise programming and help prevent injuries.
-
The general public: Even without a formal science background, basic knowledge of the ventral cavity can empower individuals to better understand their own bodies. This knowledge enables one to make informed decisions about their health and well-being.
Ultimately, the ventral cavity serves as a critical protective hub for the body’s vital organs. Grasping its organization and subdivisions unlocks a deeper comprehension of human anatomy, physiology, and clinical medicine. This understanding is essential for anyone seeking to improve their health or further their knowledge of the human body.
The Diaphragm: The Key Anatomical Separator
The ventral cavity, as we’ve explored, is a vast internal space housing a multitude of vital organs. But it isn’t just one big chamber; it’s thoughtfully divided to allow for specialized functions and protection. This division is primarily achieved by a single, incredibly important muscle: the diaphragm.
The Diaphragm: Anatomical Keystone
The diaphragm is the primary anatomical separator between the thoracic cavity, which houses the lungs and heart, and the abdominopelvic cavity, containing the digestive and reproductive organs. This dome-shaped muscle plays a pivotal role in respiration. Its unique position also dictates the boundaries of the ventral cavity’s major subdivisions.
Structure and Function: More Than Just Breathing
The diaphragm’s structure is ingeniously designed for its dual roles. It’s a broad, thin skeletal muscle that attaches to the lower ribs, the sternum, and the vertebral column.
When the diaphragm contracts, it flattens, increasing the volume of the thoracic cavity. This creates a pressure gradient that draws air into the lungs – the essential action of inhalation.
As the diaphragm relaxes, it returns to its dome shape, decreasing thoracic volume and facilitating exhalation. Beyond respiration, the diaphragm also contributes to increasing intra-abdominal pressure. This aids in processes like urination, defecation, and childbirth.
Defining the Abdominal Border
Importantly, the diaphragm’s position defines the superior border of the abdominal cavity. Everything above the diaphragm is considered part of the thoracic cavity, while everything below belongs to the abdominopelvic cavity.
This clear anatomical demarcation is crucial for medical imaging, diagnosis, and surgical planning. Understanding the diaphragm’s location allows healthcare professionals to accurately identify and assess organs within each respective cavity. It ensures that procedures and treatments are targeted effectively.
In essence, the diaphragm acts as a vital anatomical landmark. Its role in respiration and separation of the body cavities is fundamental to understanding human anatomy and physiology. Its proper function is critical for overall health.
The demarcation provided by the diaphragm is not merely an arbitrary division; it sets the stage for understanding the distinct functions and vulnerabilities of the cavities it separates. Let’s delve deeper into the thoracic cavity, exploring its intricate organization and the vital processes it safeguards.
The Thoracic Cavity: Protecting Respiration and Circulation
The thoracic cavity, a vital region within the ventral cavity, is dedicated to protecting the organs responsible for respiration and circulation.
Its bony framework, formed by the ribs, sternum, and thoracic vertebrae, provides a rigid shield against external trauma.
Understanding its boundaries and internal organization is crucial for comprehending the mechanics of breathing, blood flow, and the potential impact of various medical conditions.
Defining the Thoracic Space: Boundaries and Extent
The thoracic cavity’s boundaries are clearly defined by the skeletal structures that surround it.
Anteriorly, it is enclosed by the sternum and costal cartilages.
Posteriorly, the thoracic vertebrae form its back wall.
Laterally, the ribs curve around to complete the protective cage.
Inferiorly, the diaphragm acts as the floor, separating it from the abdominal cavity.
Superiorly, the thoracic cavity extends into the root of the neck, where structures like the trachea and esophagus pass through.
Pleural Cavities: Enclosing the Lungs
Within the thoracic cavity are the right and left pleural cavities.
Each pleural cavity surrounds a lung, providing a space for it to expand and contract during respiration.
These cavities are lined by a serous membrane called the pleura.
The pleura has two layers: the parietal pleura, which lines the inner surface of the thoracic wall, and the visceral pleura, which covers the surface of the lung.
The Role of Pleura in Reducing Friction
The pleural layers secrete a thin film of serous fluid into the pleural cavity.
This fluid acts as a lubricant, reducing friction as the lungs move during breathing.
This smooth, gliding motion is essential for efficient gas exchange.
Without this lubrication, breathing would be painful and less effective.
Pericardial Cavity: Protecting the Heart
The pericardial cavity is another crucial subdivision within the thoracic cavity.
It houses the heart, providing it with protection and allowing it to beat freely.
Location Within the Mediastinum
The pericardial cavity resides within the mediastinum, the central compartment of the thoracic cavity.
The Function of the Pericardium
The heart is enclosed within a double-layered sac called the pericardium.
The pericardium, similar to the pleura, consists of parietal and visceral layers.
The space between these layers, the pericardial cavity, contains a small amount of serous fluid.
This fluid lubricates the heart’s surface, minimizing friction as it beats.
The pericardium also helps to anchor the heart within the mediastinum and prevents it from overexpanding.
The Mediastinum: The Central Thoracic Compartment
The mediastinum is the central compartment of the thoracic cavity, located between the two pleural cavities.
Boundaries and Location
It extends from the sternum anteriorly to the vertebral column posteriorly, and from the superior thoracic aperture to the diaphragm inferiorly.
Key Structures Within the Mediastinum
The mediastinum houses a variety of vital structures, including:
- The heart and its great vessels (aorta, pulmonary artery, vena cavae).
- The trachea (windpipe).
- The esophagus.
- The thymus gland.
- Lymph nodes and nerves.
Organs of the Thoracic Cavity and Their Relationships
The primary organs within the thoracic cavity are:
- The lungs, which occupy the pleural cavities and are responsible for gas exchange.
- The heart, located within the pericardial cavity and responsible for circulating blood.
- The esophagus, which transports food from the pharynx to the stomach.
- The trachea, which carries air to the lungs.
These organs are intimately related, with the heart positioned between the lungs and the esophagus and trachea running through the mediastinum.
Their spatial arrangement is critical for their proper function and can be affected by various medical conditions.
Clinical Significance: Conditions Affecting the Thoracic Cavity
Understanding the anatomy of the thoracic cavity and its subdivisions is essential for diagnosing and treating a wide range of medical conditions.
- Pneumothorax, for example, occurs when air enters the pleural cavity, causing the lung to collapse.
- Pericarditis, inflammation of the pericardium, can restrict heart function.
- Mediastinal tumors can compress vital structures within the mediastinum.
- Pleural effusion, an abnormal accumulation of fluid in the pleural cavity, can impair breathing.
Knowledge of the location and relationships of the thoracic organs is crucial for interpreting medical imaging (X-rays, CT scans) and performing surgical procedures.
The intricate design of the thoracic cavity showcases the body’s commitment to protecting crucial respiratory and circulatory functions. Moving inferiorly past the diaphragm, we transition into another expansive region that houses a multitude of vital organs involved in digestion, excretion, and reproduction.
The Abdominopelvic Cavity: A Unified Space with Distinct Regions
The abdominopelvic cavity represents a significant portion of the ventral cavity.
It’s a large, continuous compartment that, while often discussed as two separate regions (abdominal and pelvic), functions as a single, interconnected space.
Understanding its organization is paramount for comprehending the complex interplay of organs and systems within this region.
Abdominopelvic Continuity
It’s crucial to first understand that unlike the clear separation between the thoracic and abdominal cavities provided by the diaphragm, there is no physical barrier dividing the abdominal and pelvic cavities.
This lack of separation means that structures, fluids, and even pathological processes can extend from one region to the other.
Therefore, viewing the abdominopelvic cavity as a unified entity provides a more accurate representation of its functional anatomy.
Abdominal and Pelvic Cavity Subdivisions
Despite the continuous nature of the abdominopelvic cavity, it’s convenient to divide it into two regions: the abdominal cavity and the pelvic cavity.
This distinction is primarily based on the imaginary plane that runs from the sacral promontory to the pubic symphysis.
Everything superior to this plane is generally considered the abdominal cavity, and everything inferior, the pelvic cavity.
The Abdominal Cavity: Boundaries and Contents
The abdominal cavity is the larger, superior portion of the abdominopelvic cavity.
It is bounded superiorly by the diaphragm, anteriorly by the abdominal muscles, posteriorly by the vertebral column and associated muscles, and laterally by the lower ribs and abdominal muscles.
Inferiorly, it is continuous with the pelvic cavity.
Key Abdominal Viscera
The abdominal cavity houses a diverse array of essential organs, including:
- The stomach, responsible for initial digestion.
- The liver, a major metabolic organ and producer of bile.
- The small and large intestines, crucial for nutrient absorption and waste processing.
- The spleen, which filters blood and plays a role in immune function.
- The pancreas, which produces digestive enzymes and hormones.
- The kidneys, responsible for filtering waste from the blood and regulating fluid balance.
The Peritoneal Cavity
Within the abdominal cavity lies the peritoneal cavity, a potential space lined by a serous membrane called the peritoneum.
The peritoneum has two layers: the parietal peritoneum, which lines the abdominal wall, and the visceral peritoneum, which covers the abdominal organs.
The peritoneal cavity contains a small amount of serous fluid that lubricates the surfaces of the organs, allowing them to move smoothly against each other.
Peritoneum’s Protective Role
The peritoneum plays a crucial role in supporting and protecting the abdominal organs.
It forms folds and ligaments that suspend the organs in place and provide pathways for blood vessels, nerves, and lymphatic vessels.
The peritoneum also helps to limit the spread of infection and inflammation within the abdominal cavity.
The Pelvic Cavity: Boundaries and Contents
The pelvic cavity is the smaller, inferior portion of the abdominopelvic cavity.
It is bounded anteriorly and laterally by the pelvic bones, posteriorly by the sacrum and coccyx, and inferiorly by the pelvic floor muscles.
Key Pelvic Viscera
The pelvic cavity houses several vital organs, including:
- The urinary bladder, which stores urine.
- The reproductive organs (uterus, ovaries, and fallopian tubes in females; prostate gland and seminal vesicles in males).
- The rectum, which stores feces before elimination.
Organ Relationships within the Abdominopelvic Cavity
Understanding the spatial relationships between the organs within the abdominopelvic cavity is crucial for both anatomical study and clinical practice.
For example, the proximity of the appendix to the ileum explains why appendicitis can sometimes present with symptoms similar to those of small bowel obstruction.
Similarly, the location of the kidneys near the posterior abdominal wall makes them vulnerable to injury from trauma to the back.
Clinical Significance
The abdominopelvic cavity is susceptible to a wide range of medical conditions, including:
- Infections (e.g., peritonitis, pelvic inflammatory disease).
- Inflammatory conditions (e.g., Crohn’s disease, ulcerative colitis).
- Tumors (both benign and malignant).
- Obstructions (e.g., bowel obstruction, urinary obstruction).
- Hernias.
A thorough understanding of the anatomy of the abdominopelvic cavity and its subdivisions is essential for accurate diagnosis, effective treatment planning, and successful surgical interventions.
The intricate design of the thoracic cavity showcases the body’s commitment to protecting crucial respiratory and circulatory functions. Moving inferiorly past the diaphragm, we transition into another expansive region that houses a multitude of vital organs involved in digestion, excretion, and reproduction.
Serous Membranes: The Body’s Protective Linings
Beyond the bones and muscles providing structural protection, the organs within the ventral cavity benefit from an additional layer of safeguarding: the serous membranes. These specialized tissues, including the pleura, pericardium, and peritoneum, line the internal body cavities and cover the surfaces of the organs they contain.
They play a critical role in minimizing friction, supporting organ function, and preventing the spread of infection. Understanding their structure and function is essential for grasping the overall physiology of the ventral cavity and recognizing the potential consequences of their dysfunction.
An Overview of Serous Membranes
Serous membranes are thin, double-layered structures composed of mesothelium, a type of simple squamous epithelium, and a supporting layer of connective tissue. Each membrane consists of two continuous layers: the parietal layer, which lines the cavity wall, and the visceral layer, which covers the organ.
Between these two layers is a potential space, the serous cavity, filled with a thin, watery fluid called serous fluid. This fluid is secreted by the mesothelial cells and acts as a lubricant, allowing organs to move smoothly against the cavity walls and each other.
The three primary serous membranes within the ventral cavity are:
- Pleura: Surrounds the lungs within the pleural cavities.
- Pericardium: Surrounds the heart within the pericardial cavity.
- Peritoneum: Lines the abdominal cavity and covers most of the abdominal organs.
The Function of Serous Membranes: Friction Reduction and Protection
The primary function of serous membranes is to minimize friction during movement. This is particularly important in the thoracic cavity, where the lungs expand and contract with each breath, and the heart beats continuously.
The serous fluid within the pleural and pericardial cavities reduces friction between the lungs and the chest wall, and between the heart and the surrounding structures.
This allows these organs to function efficiently without causing damage to the tissues.
In the abdominal cavity, the peritoneum performs a similar function, allowing the intestines and other organs to slide smoothly against each other during digestion and movement.
Beyond friction reduction, serous membranes also play a role in supporting and protecting the viscera.
The peritoneum, in particular, helps to hold the abdominal organs in place and prevents them from becoming tangled or displaced.
It also contains a network of blood vessels and lymphatic vessels that help to nourish and protect the abdominal organs.
Clinical Implications of Serous Membrane Inflammation
Inflammation of the serous membranes, known as serositis, can result from various causes, including infection, injury, and autoimmune diseases.
Depending on which serous membrane is affected, serositis can manifest in different ways and have significant clinical consequences.
Pleurisy (Pleuritis)
Pleurisy, or pleuritis, is inflammation of the pleura, the serous membrane lining the lungs and the thoracic cavity.
It is often caused by viral or bacterial infections, such as pneumonia or bronchitis. Symptoms of pleurisy include sharp chest pain that worsens with breathing or coughing, shortness of breath, and fever.
In some cases, pleurisy can lead to pleural effusion, an accumulation of fluid in the pleural cavity, which can further impair lung function.
Pericarditis
Pericarditis is inflammation of the pericardium, the serous membrane surrounding the heart.
It can be caused by viral or bacterial infections, autoimmune diseases, or heart attacks. Symptoms of pericarditis include chest pain, shortness of breath, and fatigue.
In severe cases, pericarditis can lead to cardiac tamponade, a life-threatening condition in which fluid accumulation in the pericardial cavity compresses the heart and impairs its ability to pump blood.
Peritonitis
Peritonitis is inflammation of the peritoneum, the serous membrane lining the abdominal cavity.
It is often caused by bacterial infection resulting from a ruptured appendix, perforated ulcer, or other abdominal trauma.
Peritonitis is a serious condition that can lead to sepsis and death if not treated promptly. Symptoms of peritonitis include severe abdominal pain, tenderness, fever, nausea, and vomiting.
The thin, lubricating serous membranes lining the body cavities are essential for reducing friction during organ movement. However, the ventral cavity is more than just a protective shell. Its anatomical layout has direct implications for diagnosing and treating a wide range of medical conditions.
Clinical Significance and Applications: Linking Anatomy to Medicine
The intricate organization of the ventral cavity isn’t merely an academic curiosity; it’s the foundation upon which clinical understanding is built. A solid grasp of the relationships between organs and their locations within these cavities is paramount for medical professionals. It impacts everything from initial diagnosis to surgical planning and postoperative care.
Anatomical Knowledge: The Cornerstone of Accurate Diagnosis
Many medical conditions manifest with symptoms localized to a specific region of the ventral cavity. Appendicitis, for instance, typically presents with pain in the lower right quadrant of the abdomen. This location directly corresponds to the anatomical position of the appendix.
Similarly, pain radiating to the left shoulder (Kehr’s sign) following abdominal trauma can indicate a ruptured spleen, reflecting referred pain pathways linked to the diaphragm.
A thorough understanding of the anatomical relationships between organs, nerves, and blood vessels is therefore critical for interpreting patient symptoms and narrowing the differential diagnosis.
Without this knowledge, clinicians may struggle to pinpoint the source of a patient’s discomfort, leading to delays in treatment and potentially adverse outcomes.
Cavity Subdivisions: Guiding Therapeutic Interventions
The subdivision of the ventral cavity into distinct regions is more than just an organizational tool for anatomists. These compartments influence how diseases spread and how treatments are administered.
For example, understanding the boundaries of the pleural cavity is essential for performing thoracentesis.
This procedure involves draining fluid from around the lungs.
Similarly, knowledge of the peritoneal cavity’s extent is crucial for managing peritonitis.
Peritonitis is a potentially life-threatening inflammation of the peritoneum.
Surgeons rely on anatomical landmarks to navigate the complex landscape of the abdominal and pelvic cavities during operations. Knowing the location of major blood vessels and nerves relative to the organs being operated on minimizes the risk of iatrogenic injury.
Visceral Health: A Reflection of Overall Well-being
The organs housed within the ventral cavity—the viscera—are central to numerous physiological processes. Consequently, their health directly impacts overall well-being. Conditions affecting the viscera, such as liver cirrhosis, inflammatory bowel disease, or kidney failure, can have widespread systemic effects.
Understanding the anatomical relationships between these organs allows clinicians to predict the potential consequences of visceral dysfunction and to tailor treatment strategies accordingly.
For example, portal hypertension secondary to liver disease can lead to the formation of esophageal varices, posing a risk of life-threatening bleeding. Recognition of this connection allows for prophylactic interventions to prevent variceal rupture.
In essence, the health of the viscera within the ventral cavity serves as a barometer for overall health.
By appreciating the anatomical context in which these organs function, medical professionals can provide more effective and holistic care.
Ventral Cavity Subdivisions: Frequently Asked Questions
Here are some frequently asked questions about the ventral cavity and its subdivisions to further clarify its anatomy.
What are the main subdivisions of the ventral cavity?
The ventral cavity is broadly divided into two main cavities: the thoracic cavity and the abdominopelvic cavity. These ventral cavity subdivisions are separated by the diaphragm.
What organs are located in the thoracic cavity?
The thoracic cavity primarily houses the lungs, heart, trachea, esophagus, and major blood vessels. It is a protected space vital for respiration and circulation, enclosed by the rib cage.
What is the difference between the abdominal and pelvic cavities?
The abdominal cavity contains organs like the stomach, intestines, liver, pancreas, and kidneys. The pelvic cavity, which lies inferior to the abdominal cavity, houses the bladder, reproductive organs, and rectum. These are important distinctions within the ventral cavity subdivisions.
What membranes line the ventral cavity and its subdivisions?
The ventral cavity and its subdivisions are lined with serous membranes, specifically the parietal and visceral layers. These membranes secrete serous fluid, reducing friction and allowing organs to move smoothly within the ventral cavity.
So, that wraps up our deep dive into ventral cavity subdivisions! Hopefully, this guide has given you a better grasp of these important anatomical regions. Good luck with your studies, and remember to keep exploring the fascinating world of anatomy!