Understanding the structure of HB requires a comprehensive analysis of its interconnected components. Human behavioral science provides the foundational principles for interpreting these frameworks. Successful application often necessitates the careful consideration of organizational culture. Furthermore, advanced analytical tools such as system dynamics modeling, aid in visualizing and optimizing the structure of HB for better outcomes, which improves understanding of individual well-being.
Hemoglobin (Hb), the protein that lends blood its crimson hue, is far more than just a pigment. It is the linchpin of oxygen transport throughout the body, a sophisticated molecular machine that ensures every cell receives the life-sustaining energy it needs. Understanding its intricate structure is not merely an academic exercise.
It is the key to unlocking a deeper comprehension of its function, its vulnerabilities, and the devastating consequences that arise when its architecture is compromised.
Hemoglobin: The Body’s Oxygen Courier
At its core, hemoglobin is a protein found in red blood cells. Its primary function is to bind to oxygen in the lungs and ferry it to tissues throughout the body. Without hemoglobin, our cells would be starved of oxygen. Cellular processes would grind to a halt.
Life as we know it would be impossible.
The Importance of Structural Understanding
The efficiency and reliability of hemoglobin depend entirely on its precise three-dimensional structure. This structure dictates how readily hemoglobin binds to oxygen, how it responds to changes in its environment, and how it releases oxygen where it is needed most.
When this structure is disrupted, the consequences can be dire.
The Roadmap Ahead: A Comprehensive Overview
This guide provides a comprehensive exploration of hemoglobin’s structural intricacies. We will dissect its components, examine the mechanisms that govern its function, and delve into the devastating impact of structural abnormalities.
From the building blocks of globin chains to the subtle interplay of regulatory molecules, we aim to shed light on this remarkable molecule and its profound significance for human health.
Our journey will encompass:
- The fundamental architecture of the hemoglobin molecule.
- The delicate balance between structure and function.
- The pathologies that arise when this balance is disrupted.
- The future of research and treatment in hemoglobin-related disorders.
Hemoglobin: The Body’s Oxygen Courier
At its core, hemoglobin is a protein found in red blood cells. Its primary function is to bind to oxygen in the lungs and ferry it to tissues throughout the body. Without hemoglobin, our cells would be starved of oxygen. Cellular processes would grind to a halt. Life as we know it would be impossible.
The Importance of Structural Understanding
The efficiency and reliability of hemoglobin depend entirely on its precise three-dimensional structure. This structure dictates how readily hemoglobin binds to oxygen, how it responds to changes in its environment, and how it releases oxygen where it is needed most. When this structure is disrupted, the consequences can be dire.
With a firm grasp of why hemoglobin’s structure is so crucial, let’s delve into the specific molecular components that comprise this remarkable protein. Understanding these building blocks is essential to appreciating the complexity and elegance of its function.
The Molecular Architecture: Building Blocks of Hemoglobin
Hemoglobin’s function as an oxygen carrier is intrinsically linked to its complex architecture. It isn’t a simple, monolithic structure, but rather a carefully constructed assembly of smaller components, each playing a vital role in its overall function. Let’s dissect these fundamental building blocks.
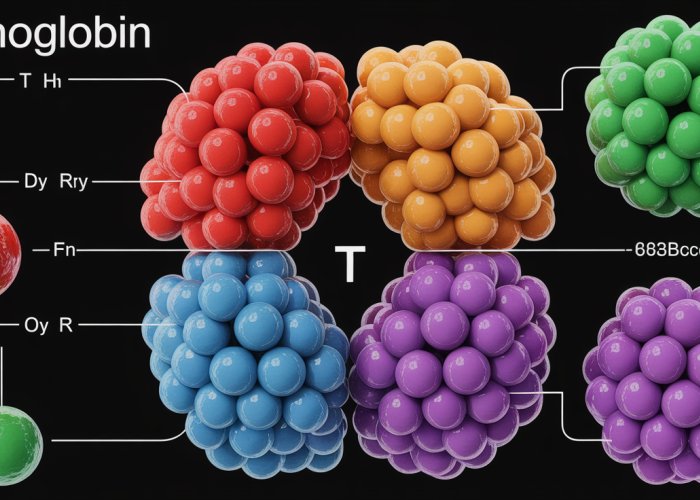
The Tetrameric Assembly: Four Subunits United
Hemoglobin is a tetramer, meaning it’s comprised of four protein subunits. These subunits are not identical. The most common form of adult hemoglobin, known as hemoglobin A (HbA), consists of two alpha (α) globin chains and two beta (β) globin chains.
This quaternary structure – the specific arrangement of these subunits in three-dimensional space – is crucial. It allows for cooperative binding, meaning the binding of oxygen to one subunit increases the affinity of the other subunits for oxygen.
Alpha and Beta Globin Chains: The Protein Scaffolding
The alpha and beta globin chains are polypeptide chains, sequences of amino acids linked together. While they differ in their specific amino acid sequence, both alpha and beta globin chains share a similar overall structure, known as the globin fold. This fold creates a pocket that cradles a critical component: the heme group.
Different hemoglobin variants exist, such as Hemoglobin F (HbF), the primary oxygen carrier in fetal blood. HbF replaces the beta chains with gamma chains.
Alpha Globin: Characteristics and Genetic Encoding
The alpha globin gene cluster is located on chromosome 16. Humans typically have two copies of the alpha-globin gene on each chromosome, totaling four alpha-globin genes. This redundancy is important because defects in alpha-globin production can lead to alpha-thalassemia.
Beta Globin: Characteristics and Genetic Encoding
The beta globin gene is located on chromosome 11. Unlike alpha globin, there is only one beta-globin gene on each chromosome, totaling two beta-globin genes. Mutations in the beta-globin gene can cause beta-thalassemia or sickle cell anemia, emphasizing the critical role of this single gene.
The Heme Group: The Oxygen-Binding Site
At the heart of each globin chain lies the heme group. This is a porphyrin ring, a complex organic molecule with a central iron (Fe) atom. The heme group is the functional center of hemoglobin, as it is the site where oxygen actually binds. Without the heme group, hemoglobin would be unable to carry oxygen.
The structure of the porphyrin ring is meticulously arranged to create an ideal environment for iron to bind oxygen reversibly.
Iron and Oxygen: A Delicate Dance
The iron atom within the heme group exists in the ferrous (Fe2+) state. In this state, it can readily bind to oxygen. This binding is not permanent. Oxygen binds reversibly to the iron atom, allowing hemoglobin to pick up oxygen in the lungs (where oxygen concentration is high) and release it in the tissues (where oxygen concentration is low).
This reversible binding is essential for oxygen delivery to the body.
The Role of Iron Oxidation State
If the iron atom were to be oxidized to the ferric (Fe3+) state, it would be unable to bind oxygen. Hemoglobin containing ferric iron is called methemoglobin and is non-functional for oxygen transport. The body has mechanisms to prevent the oxidation of iron in hemoglobin.
Hemoglobin’s function as an oxygen carrier is intrinsically linked to its complex architecture. It isn’t a simple, monolithic structure, but rather a carefully constructed assembly of smaller components, each playing a vital role in its overall function. Let’s dissect these fundamental building blocks.
Structure-Function Relationship: Decoding Hemoglobin’s Efficiency
The true marvel of hemoglobin lies not just in its constituent parts, but in how these parts interact to achieve efficient oxygen transport. The protein’s effectiveness is deeply rooted in its dynamic quaternary structure and its responsiveness to subtle changes in its physiological environment. This section explores how hemoglobin’s structure dictates its function, and how factors like pH, carbon dioxide, and 2,3-BPG fine-tune its oxygen affinity.
The Significance of Quaternary Structure
Hemoglobin’s quaternary structure, the arrangement of its four subunits (two α-globin and two β-globin chains) in three-dimensional space, is critical to its function. This arrangement facilitates cooperative binding, a phenomenon where the binding of one oxygen molecule to a heme group increases the affinity of the remaining heme groups for oxygen.
This cooperativity is essential for efficient oxygen loading in the lungs, where oxygen concentration is high, and unloading in the tissues, where oxygen concentration is low. Without this cooperative interaction, hemoglobin’s oxygen-carrying capacity would be significantly diminished.
The protein exists in two primary states: the T (tense) state, which has a lower affinity for oxygen, and the R (relaxed) state, which has a higher affinity. Oxygen binding triggers a conformational change that shifts the equilibrium from the T state to the R state, further enhancing oxygen uptake.
The Bohr Effect: Environmental Influence on Oxygen Binding
The Bohr effect describes the relationship between pH and carbon dioxide concentration and hemoglobin’s affinity for oxygen. In essence, a decrease in pH (increased acidity) or an increase in carbon dioxide concentration promotes oxygen release from hemoglobin.
This phenomenon is particularly important in metabolically active tissues, where both carbon dioxide production and acidity are elevated. The increased carbon dioxide concentration stabilizes the T state of hemoglobin, reducing its oxygen affinity and facilitating oxygen delivery to the tissues that need it most.
Conversely, in the lungs, where carbon dioxide concentration is low and pH is relatively high, hemoglobin’s affinity for oxygen increases, promoting efficient oxygen uptake. The Bohr effect, therefore, represents a crucial mechanism for matching oxygen supply with oxygen demand.
2,3-Bisphosphoglycerate (2,3-BPG): Fine-Tuning Oxygen Affinity
2,3-Bisphosphoglycerate (2,3-BPG) is a molecule found in red blood cells that plays a critical role in regulating hemoglobin’s oxygen affinity. It binds to deoxyhemoglobin, preferentially stabilizing the T state and reducing hemoglobin’s affinity for oxygen.
The concentration of 2,3-BPG increases under conditions of hypoxia, such as at high altitude or in individuals with chronic lung disease. The increased 2,3-BPG levels cause hemoglobin to release more oxygen to the tissues, compensating for the reduced oxygen availability.
2,3-BPG essentially acts as a negative allosteric effector, fine-tuning hemoglobin’s oxygen-binding properties to meet the body’s physiological needs. This adaptation ensures that tissues receive an adequate supply of oxygen, even under challenging conditions.
When Structure Fails: Hemoglobinopathies and Their Impact
We’ve seen how meticulously crafted hemoglobin’s structure is, with each component precisely arranged to facilitate efficient oxygen transport. But what happens when this delicate architecture is compromised? The consequences can be profound, leading to a class of disorders known as hemoglobinopathies.
These conditions arise from genetic mutations that disrupt either the structure or the production of globin chains, impacting hemoglobin’s ability to function correctly. Let’s explore two prominent examples: Sickle Cell Anemia and Thalassemia, each showcasing the devastating effects of structural defects on hemoglobin’s function and overall health.
The Impact of Structural Defects
Structural abnormalities in hemoglobin can manifest in various ways, ultimately affecting its ability to bind, transport, and release oxygen. These defects can alter the protein’s stability, solubility, or its interaction with other molecules, leading to a cascade of adverse effects.
A seemingly small alteration in the amino acid sequence can trigger significant changes in the protein’s three-dimensional structure, disrupting its delicate equilibrium and impairing its function. The severity of the impact depends on the nature and location of the mutation, as well as the individual’s genetic background.
Sickle Cell Anemia: A Molecular Misstep
Sickle Cell Anemia is perhaps the most well-known hemoglobinopathy, a stark reminder of how a single point mutation can have devastating consequences.
The Genetic Basis
This genetic disorder arises from a mutation in the β-globin gene, where a single nucleotide substitution leads to the replacement of glutamic acid with valine at the sixth position of the β-globin chain. This seemingly minor change has profound effects on hemoglobin’s structure and function.
The Sickling Phenomenon
The altered hemoglobin, termed hemoglobin S (HbS), has a tendency to polymerize under low oxygen conditions, forming long, rigid fibers inside red blood cells. This polymerization distorts the cells into a characteristic sickle shape, hence the name Sickle Cell Anemia.
Clinical Consequences
These sickled red blood cells are less flexible than normal cells and have difficulty passing through small blood vessels. This leads to vaso-occlusion, causing pain crises, tissue damage, and organ dysfunction. Chronic hemolysis (destruction of red blood cells) also results in anemia, fatigue, and other complications.
A Cascade of Complications
The chronic inflammation and vascular damage associated with Sickle Cell Anemia can affect virtually every organ system in the body, leading to a reduced lifespan and significant morbidity.
Thalassemia: An Imbalance in Production
Unlike Sickle Cell Anemia, which results from a structural defect, Thalassemia arises from a quantitative deficiency in globin chain production. This imbalance disrupts the normal tetrameric structure of hemoglobin, leading to a variety of clinical manifestations.
Types of Thalassemia
Thalassemia is broadly classified into α-thalassemia and β-thalassemia, depending on which globin chain is affected. α-thalassemia results from reduced or absent production of α-globin chains, while β-thalassemia is caused by a deficiency in β-globin chain synthesis.
The Consequences of Imbalance
In both types of thalassemia, the deficiency of one globin chain leads to an excess of the other. This excess chain can form insoluble aggregates that damage red blood cell precursors in the bone marrow, leading to ineffective erythropoiesis (red blood cell production) and anemia.
Clinical Variability
The severity of thalassemia varies widely, depending on the specific genetic mutations involved and the degree of globin chain deficiency. Some individuals may be asymptomatic carriers, while others may require lifelong blood transfusions and other medical interventions.
Impact on Hemoglobin Function
In addition to causing anemia, thalassemia can also affect hemoglobin’s oxygen-carrying capacity and its ability to release oxygen to tissues. The abnormal hemoglobin tetramers formed in thalassemia are often unstable and have altered oxygen affinity, further contributing to the clinical manifestations of the disease.
The Broader Implications: Benefits of Understanding Hemoglobin Structure
The intricate world of hemoglobin structure extends far beyond the laboratory bench. A deep understanding of its architecture unlocks critical insights for medical professionals and genetics researchers alike, impacting diagnostics, treatment strategies, and the very frontiers of scientific knowledge.
Enhancing Medical Practice: Diagnostics and Treatment
For medical professionals, a solid grasp of hemoglobin structure is not merely academic; it’s a fundamental tool in the diagnosis and management of a range of diseases.
Understanding the subtle nuances of hemoglobin’s conformation, its affinity for oxygen under varying physiological conditions, and the impact of mutations allows for more accurate interpretation of diagnostic tests.
Diagnostic Accuracy
For example, in cases of suspected hemoglobinopathies, knowledge of the specific structural defects associated with different variants is crucial for accurate identification.
High-performance liquid chromatography (HPLC) and electrophoresis techniques rely on the structural differences of various hemoglobin types to separate and quantify them, providing critical diagnostic information.
Furthermore, understanding the structure-function relationship enables clinicians to predict the clinical course of certain hemoglobinopathies. This allows for proactive intervention and personalized treatment plans.
Tailored Treatment Strategies
Knowledge of how specific structural defects affect oxygen binding and delivery allows for more targeted therapeutic interventions. For instance, understanding the mechanism by which hydroxyurea increases fetal hemoglobin (HbF) production in sickle cell anemia guides its use in mitigating the severity of the disease.
Similarly, insights into the structural basis of hemoglobin instability can inform the use of antioxidants or other therapies aimed at preventing oxidative damage.
Furthermore, advancements in gene therapy and CRISPR-Cas9 technology hold immense promise for correcting the underlying genetic defects that cause hemoglobinopathies. These approaches are predicated on a precise understanding of the globin gene structure and the consequences of its mutations.
Fueling Genetics Research: Unraveling Hemoglobinopathies
For genetics researchers, hemoglobin serves as a model system for studying the relationship between gene mutations, protein structure, and disease phenotype.
The relatively simple genetic architecture of hemoglobin, with its well-defined alpha and beta globin genes, makes it an ideal target for investigating the molecular basis of genetic disorders.
Advancing Knowledge of Hemoglobinopathies
Research into hemoglobin structure has been instrumental in identifying and characterizing hundreds of different hemoglobin variants, each with its unique structural and functional properties.
These studies have provided invaluable insights into the mechanisms by which mutations can disrupt protein folding, stability, and function, leading to a wide spectrum of clinical manifestations.
Pushing the Boundaries of Research
Moreover, the ongoing quest to understand hemoglobin structure is driving the development of new technologies and approaches for studying protein structure and function.
Cryo-electron microscopy (cryo-EM) and X-ray crystallography, for example, have been used to determine the three-dimensional structures of hemoglobin variants at atomic resolution, providing unprecedented detail into their molecular architecture.
The knowledge gained from these studies is not only advancing our understanding of hemoglobinopathies but also informing research into other protein-related diseases.
The continued exploration of hemoglobin structure promises to unlock further therapeutic avenues and deepen our understanding of human genetics and disease.
FAQs: Understanding HB Structures and Benefits
These frequently asked questions clarify key aspects of HB structures and their associated benefits.
What exactly is an HB structure and why is it important?
An HB structure, in the context of benefits, refers to the organizational framework that defines how benefits are designed, administered, and delivered to employees. Understanding the structure of hb is critical for both employers and employees. A well-defined structure ensures fair access, efficient management, and optimal utilization of offered benefits.
How does the structure of hb affect the benefits I receive?
The specific structure of hb determines eligibility criteria, coverage levels, and the processes for accessing different benefits. A decentralized structure, for example, might offer more localized or customizable benefits, while a centralized one may prioritize cost-effectiveness and standardization. Understanding the underlying structure helps employees navigate their benefit options more effectively.
What are the key components of a typical HB structure?
A typical HB structure involves defining eligible employees, benefit tiers (if any), provider networks, contribution strategies (employee vs. employer), and communication channels. A clear structure of hb also includes established procedures for enrollment, claims processing, and resolving disputes.
How can I learn more about the specific HB structure at my company?
Your company’s HR department is the primary source for information on the structure of hb in place. You can usually find details in the employee handbook, benefits portal, or through scheduled meetings with HR representatives. Don’t hesitate to ask questions for clarification.
So, there you have it – a peek into the world of structure of HB! Hopefully, this guide has given you a solid foundation. Now go explore and put that knowledge to good use!