Understanding smooth muscle characteristics is fundamental in grasping the intricate functions of various physiological systems. Contractility, a key property, allows smooth muscle to generate force within organs like the gastrointestinal tract. Its regulation is influenced by a multitude of factors, including the autonomic nervous system, which modulates smooth muscle activity without conscious control. Furthermore, the research conducted at institutions like the Mayo Clinic continually expands our knowledge of how disturbances in these smooth muscle characteristics contribute to different medical conditions. Finally, advances in electrophysiology help us to better understand the electrical properties of smooth muscles.
The human body is a marvel of coordinated activity, orchestrated by a diverse array of tissues, each with specialized functions. Among these, muscle tissue plays a pivotal role in movement, stability, and a host of involuntary processes essential for life.
There are three distinct types of muscle tissue: skeletal, cardiac, and smooth muscle. While skeletal muscle enables voluntary movements like walking and lifting, and cardiac muscle tirelessly pumps blood throughout our circulatory system, smooth muscle operates largely behind the scenes, yet its influence is profound and pervasive.
A Trio of Muscle Tissues
Let’s briefly touch upon the defining characteristics of each muscle type:
-
Skeletal muscle, as the name suggests, is attached to bones and responsible for voluntary movement. Its cells are striated, meaning they have a striped appearance under a microscope, and are multinucleated.
-
Cardiac muscle is found exclusively in the heart. Like skeletal muscle, it is striated, but its cells are branched and connected by specialized junctions called intercalated discs, allowing for coordinated contractions.
-
Smooth muscle, our primary focus, lacks the striations of the other two types, hence its name. It is found in the walls of internal organs and blood vessels, where it controls involuntary movements like digestion, blood pressure regulation, and uterine contractions.
The Ubiquitous Nature of Smooth Muscle
Smooth muscle is far more widespread than many realize. It lines the walls of blood vessels, regulating blood pressure and flow.
It propels food through the digestive tract via peristalsis, controls the diameter of airways in the lungs, and governs the expulsion of urine from the bladder.
In the uterus, it orchestrates the powerful contractions of childbirth.
Its pervasive presence underscores its critical role in maintaining homeostasis and ensuring the proper functioning of numerous organ systems.
Thesis Statement
This guide will serve as a comprehensive exploration into the fascinating world of smooth muscle. We will delve into its unique structural and functional characteristics, providing an in-depth understanding of its vital role in various physiological processes.
By examining its cellular organization, contraction mechanisms, regulatory controls, and diverse functions, we aim to shed light on this often-overlooked yet indispensable tissue.
The scope of smooth muscle extends far beyond mere presence; its function is inextricably linked to its unique structure. Understanding its architecture at the microscopic level is critical to appreciating how this tissue orchestrates so many vital, involuntary processes.
Structural Characteristics: A Microscopic View
To fully appreciate the functionality of smooth muscle, we must first delve into its microscopic architecture. From its cellular arrangement to the organization of its contractile filaments and the communication networks between cells, the structure of smooth muscle is uniquely suited to its role in regulating involuntary bodily functions.
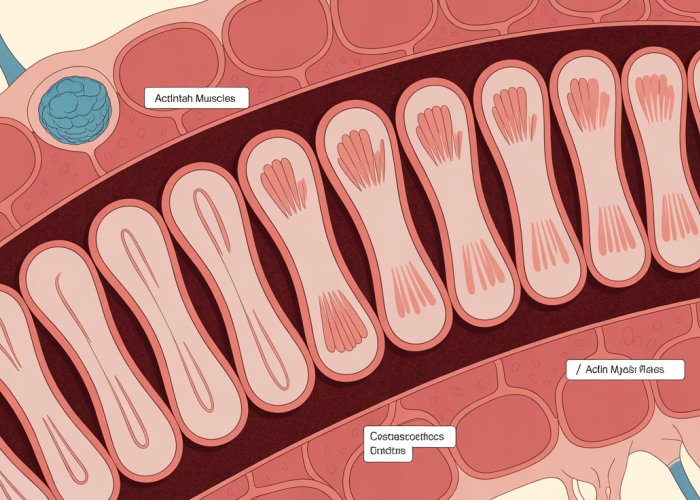
Cellular Organization: A Spindle-Shaped Symphony
Unlike the long, cylindrical, multinucleated fibers of skeletal muscle, smooth muscle cells are spindle-shaped, tapering at both ends.
These individual cells, typically ranging from 20 to 500 micrometers in length, are arranged in sheets or bundles, often oriented in multiple directions.
This arrangement allows for contraction in various planes, crucial for functions like peristalsis in the digestive tract or constriction of blood vessels.
The Absence of Striations: Defining "Smooth"
A defining characteristic of smooth muscle is the absence of striations, the characteristic striped pattern seen in skeletal and cardiac muscle. This is due to the less organized arrangement of actin and myosin filaments compared to the highly structured sarcomeres found in striated muscle.
This lack of striations is, in fact, where the name "smooth" muscle originates.
The arrangement, or lack thereof, directly informs the style of contraction.
The Singular Nucleus: A Central Command
Each smooth muscle cell contains a single, centrally located nucleus.
This contrasts sharply with the multinucleated nature of skeletal muscle fibers.
The single nucleus houses the genetic material necessary for protein synthesis and cellular maintenance, orchestrating the cell’s activities from its central position.
Filament Organization: A Web of Contractile Proteins
The contractile force in smooth muscle is generated by the interaction of actin and myosin filaments, similar to skeletal muscle.
However, the organization of these filaments differs significantly.
Instead of being arranged into sarcomeres, actin and myosin filaments are dispersed throughout the cytoplasm, forming a web-like network.
Dense Bodies: Anchoring the Network
A key feature of smooth muscle is the presence of dense bodies.
These protein structures, analogous to the Z-discs in skeletal muscle, serve as attachment points for actin filaments.
Dense bodies are found both within the cytoplasm and attached to the cell membrane, providing a structural framework for contraction.
Think of dense bodies as the connective knots holding together the interwoven threads of a complex tapestry.
Actin to Myosin Ratio: Efficiency in Sustained Contraction
The ratio of actin to myosin filaments is significantly higher in smooth muscle (10-15:1) than in skeletal muscle (2:1).
This higher ratio allows for greater cross-bridge formation and sustained contraction with less energy expenditure, which is ideal for maintaining prolonged tone in blood vessels or the digestive tract.
The efficiency is key to its function.
Cell Communication: The Role of Gap Junctions
Smooth muscle cells communicate with each other through gap junctions.
These specialized channels allow for the direct passage of ions and small molecules between adjacent cells, facilitating the rapid spread of electrical signals and coordinated contraction.
Gap Junctions in Visceral Smooth Muscle: A Symphony of Synchronization
Gap junctions are particularly abundant in visceral smooth muscle, the type found in the walls of internal organs like the digestive tract and uterus.
This extensive network of gap junctions allows for the synchronized contraction of large groups of cells, essential for peristalsis and other coordinated movements.
The function directly ties into the structure.
Modulation of Gap Junction Activity: Fine-Tuning Communication
The activity of gap junctions can be modulated by various factors, including neurotransmitters, hormones, and local mediators.
This modulation allows for fine-tuning of smooth muscle activity in response to changing physiological conditions.
The regulation of gap junction activity is complex.
Structural subtleties lay the foundation, but the true magic of smooth muscle lies in its ability to contract and relax, orchestrating vital functions with remarkable efficiency. This dynamic process is a carefully choreographed interplay of molecular events, distinct from the mechanics of striated muscle, enabling sustained contractions with minimal energy expenditure.
Functional Characteristics: Contraction and Relaxation Mechanisms
Smooth muscle contraction and relaxation are complex processes regulated by a variety of factors. Understanding these mechanisms is crucial for comprehending how smooth muscle performs its diverse functions throughout the body.
Excitation-Contraction Coupling: The Spark of Contraction
Excitation-contraction coupling in smooth muscle differs significantly from that in skeletal muscle. The process is initiated by an increase in intracellular calcium ion (Ca2+) concentration.
This increase can occur through two primary pathways: influx of Ca2+ from the extracellular space via voltage-gated or ligand-gated channels, and release of Ca2+ from the sarcoplasmic reticulum (SR), an intracellular storage site.
The Role of Calcium Ions (Ca2+)
Calcium ions serve as the primary trigger for smooth muscle contraction. The source of these ions, whether from outside the cell or from internal stores, is critical to the specific contractile response.
Calmodulin Activation: The Calcium Sensor
Once inside the cell, Ca2+ binds to calmodulin, a calcium-binding protein. This binding activates calmodulin, initiating a downstream signaling cascade.
Myosin Light Chain Kinase (MLCK): The Key Enzyme
The calcium-calmodulin complex then activates myosin light chain kinase (MLCK). MLCK is an enzyme that phosphorylates the myosin light chain, a component of the myosin protein.
Phosphorylation of the myosin light chain is a crucial step, enabling myosin to interact with actin and initiate cross-bridge cycling.
The Sliding Filament Mechanism in Smooth Muscle
Smooth muscle contraction relies on the sliding filament mechanism, similar to skeletal muscle, but with key differences.
Phosphorylated Myosin and Actin Interaction
Phosphorylated myosin can now bind to actin filaments. This interaction forms cross-bridges, which generate force and cause the filaments to slide past each other, leading to contraction.
Cross-Bridge Cycling and Force Generation
The cycling of these cross-bridges, powered by ATP hydrolysis, results in the shortening of the smooth muscle cell. This generates tension and causes the contraction.
Comparison to Skeletal Muscle Contraction
While both smooth and skeletal muscle utilize the sliding filament mechanism, the arrangement of actin and myosin filaments differs.
Smooth muscle lacks the highly organized sarcomeric structure found in skeletal muscle, contributing to its unique contractile properties.
Relaxation: Returning to the Resting State
Smooth muscle relaxation occurs when the intracellular calcium ion concentration decreases. This leads to the deactivation of the pathways that initiate contraction.
Decreasing Intracellular Calcium Ions (Ca2+)
The reduction in Ca2+ levels can be achieved through several mechanisms, including pumping Ca2+ back into the sarcoplasmic reticulum or out of the cell via Ca2+ pumps and exchangers.
Myosin Light Chain Phosphatase (MLCP): Reversing the Process
Myosin light chain phosphatase (MLCP) plays a critical role in relaxation. MLCP dephosphorylates the myosin light chain, reducing myosin ATPase activity and preventing further cross-bridge cycling.
Signaling Pathways Promoting Relaxation
Various signaling pathways, such as those involving nitric oxide (NO) and cyclic GMP (cGMP), can also promote smooth muscle relaxation by influencing calcium levels and MLCP activity.
The Latch State: Sustained Contraction with Minimal Energy
Smooth muscle exhibits a unique characteristic known as the latch state, which allows it to maintain prolonged contractions with minimal energy expenditure.
Description and Significance of the Latch State
In the latch state, myosin cross-bridges remain attached to actin for an extended period. This sustains tension without requiring continuous ATP hydrolysis.
Mechanisms Involved in Maintaining the Latch State
The precise mechanisms underlying the latch state are not fully understood, but it is believed to involve a decreased rate of cross-bridge detachment and a prolonged attachment of dephosphorylated myosin to actin.
Importance in Maintaining Tone
The latch state is particularly important in maintaining tone in blood vessels and other organs, allowing them to sustain contraction over long periods without fatigue. This is vital for regulating blood pressure and maintaining organ function.
Structural subtleties lay the foundation, but the true magic of smooth muscle lies in its ability to contract and relax, orchestrating vital functions with remarkable efficiency. This dynamic process is a carefully choreographed interplay of molecular events, distinct from the mechanics of striated muscle, enabling sustained contractions with minimal energy expenditure. All these processes are vital, but the final act involves the body’s intricate regulatory mechanisms that fine-tune smooth muscle activity, ensuring optimal physiological function.
Regulation of Smooth Muscle Activity
Smooth muscle activity is far from a simple on-off switch. It’s a nuanced, finely tuned process influenced by a symphony of signals originating from the autonomic nervous system, circulating hormones, and localized paracrine factors. This multifaceted regulation is crucial for maintaining homeostasis and responding to varying physiological demands.
The Autonomic Nervous System’s Influence
The autonomic nervous system (ANS), the body’s involuntary control network, exerts significant influence over smooth muscle activity. Both the sympathetic and parasympathetic branches of the ANS innervate smooth muscle, releasing neurotransmitters that either stimulate or inhibit contraction.
Sympathetic Innervation: The sympathetic nervous system, often associated with the "fight or flight" response, generally promotes smooth muscle relaxation in certain areas, such as the airways, and contraction in others, like blood vessels. This divergence is mediated by different adrenergic receptors on the smooth muscle cells. For example, norepinephrine, the primary sympathetic neurotransmitter, can bind to α-adrenergic receptors to cause vasoconstriction or to β-adrenergic receptors to induce bronchodilation.
Parasympathetic Innervation: Conversely, the parasympathetic nervous system, responsible for "rest and digest" functions, typically promotes smooth muscle contraction in the digestive tract and relaxation in blood vessels supplying skeletal muscle. Acetylcholine (ACh) is the primary neurotransmitter released by parasympathetic nerve fibers. ACh binds to muscarinic receptors on smooth muscle cells, triggering a cascade of intracellular events that lead to contraction.
The effects of neurotransmitters are not uniform across all smooth muscle types.
The specific response depends on the type of receptor present on the smooth muscle cell and the intracellular signaling pathways activated upon receptor binding.
Hormonal Control
Hormones, chemical messengers secreted by endocrine glands, also play a vital role in modulating smooth muscle activity. These hormones can exert their effects by binding to receptors on the smooth muscle cell membrane or by entering the cell and interacting with intracellular receptors.
Examples of Hormonal Influence:
Several hormones influence smooth muscle.
For example, epinephrine (adrenaline), released from the adrenal medulla, can cause bronchodilation or vasoconstriction depending on the receptor type. Angiotensin II, a potent vasoconstrictor, plays a crucial role in regulating blood pressure. Oxytocin, released during childbirth, stimulates uterine smooth muscle contraction.
Mechanisms of Hormonal Action: Hormones can act through various mechanisms, including:
- Modulating intracellular calcium levels.
- Altering the sensitivity of the contractile machinery to calcium.
- Influencing the activity of myosin light chain kinase (MLCK) and myosin light chain phosphatase (MLCP).
- Regulating gene expression to alter the synthesis of contractile proteins.
The response to hormonal stimulation is influenced by the receptor density on the smooth muscle cell, the affinity of the hormone for its receptor, and the downstream signaling pathways activated.
Local Factors
In addition to neural and hormonal control, smooth muscle activity is also regulated by local factors within the tissue microenvironment. These factors include paracrine signaling molecules, metabolites, and physical stimuli.
Paracrine Signaling: Paracrine signaling involves the release of signaling molecules from cells that act on neighboring cells.
Examples of paracrine factors that affect smooth muscle include:
- Nitric oxide (NO), a potent vasodilator.
- Prostaglandins, which can either contract or relax smooth muscle depending on the specific prostaglandin and receptor subtype.
- Endothelin-1, a powerful vasoconstrictor.
These paracrine factors are often released in response to changes in the local environment, such as inflammation, tissue damage, or changes in blood flow.
Influence of Metabolites:
Changes in the concentration of metabolites, such as oxygen, carbon dioxide, hydrogen ions (pH), and adenosine, can also affect smooth muscle tone. For example, a decrease in oxygen tension can cause vasodilation in certain vascular beds, while an increase in carbon dioxide can lead to bronchodilation. These local metabolic responses help to match blood flow and airflow to the metabolic demands of the tissue.
The interplay between the autonomic nervous system, hormones, and local factors creates a complex regulatory network that ensures smooth muscle activity is precisely controlled to meet the ever-changing demands of the body. Understanding these regulatory mechanisms is essential for developing effective treatments for a wide range of diseases involving smooth muscle dysfunction.
Smooth Muscle in Different Organ Systems: A Symphony of Functions
Having explored the intricate mechanisms that govern smooth muscle activity, it’s time to appreciate the diverse roles this tissue plays across various organ systems. From the rhythmic contractions of the digestive tract to the precise control of blood vessel diameter, smooth muscle orchestrates a symphony of functions essential for life.
Blood Vessels: The Guardians of Blood Pressure
Smooth muscle within the walls of blood vessels is critical for regulating blood pressure and ensuring efficient blood flow.
This control is primarily achieved through vasoconstriction (narrowing of blood vessels) and vasodilation (widening of blood vessels).
Vasoconstriction, driven by smooth muscle contraction, increases resistance to blood flow, thereby raising blood pressure.
Conversely, vasodilation, resulting from smooth muscle relaxation, reduces resistance and lowers blood pressure.
This dynamic interplay allows the body to adapt to changing physiological demands, such as exercise or changes in posture, ensuring that tissues receive adequate oxygen and nutrients.
Digestive Tract: Peristalsis and the Rhythm of Digestion
Within the digestive tract, smooth muscle is responsible for peristalsis, the rhythmic waves of contraction that propel food along the gastrointestinal tract.
This coordinated movement ensures that food is properly mixed with digestive enzymes and efficiently absorbed.
Sphincters, specialized rings of smooth muscle, control the passage of food between different segments of the digestive tract, preventing backflow and regulating the rate of digestion.
The precise timing and coordination of these contractions are essential for efficient digestion and nutrient absorption.
Urinary Bladder: Orchestrating Micturition
The urinary bladder relies on smooth muscle to control the storage and release of urine.
As the bladder fills, smooth muscle in its wall (detrusor muscle) relaxes to accommodate the increasing volume.
During micturition (urination), the detrusor muscle contracts, increasing pressure within the bladder and forcing urine out through the urethra.
The process is tightly regulated by the nervous system, ensuring voluntary control over urination.
Uterus: The Power of Contraction During Childbirth
The uterus, a dynamic organ capable of dramatic changes, relies heavily on smooth muscle.
During pregnancy, uterine smooth muscle undergoes significant growth and remodeling.
As labor approaches, the sensitivity of uterine smooth muscle to various stimuli increases, leading to coordinated contractions that expel the fetus during childbirth.
The intensity and frequency of these contractions are precisely regulated by hormones and local factors, ensuring a safe and effective delivery.
Lungs: The Gatekeepers of Airflow
In the lungs, smooth muscle controls the diameter of the airways, regulating airflow during breathing.
Bronchodilation, the widening of the airways, is facilitated by smooth muscle relaxation, allowing for increased airflow during exercise or periods of increased oxygen demand.
Conversely, bronchoconstriction, the narrowing of the airways, is caused by smooth muscle contraction, which can occur in response to irritants or allergens.
This delicate balance is essential for maintaining optimal respiratory function.
Visceral vs. Multi-Unit Smooth Muscle: Two Styles of Contraction
Smooth muscle is not a monolithic entity; it exists in two primary forms: visceral and multi-unit.
Visceral smooth muscle, found in the walls of many internal organs (e.g., digestive tract, uterus), is characterized by coordinated contractions due to the presence of gap junctions.
These junctions allow for the rapid spread of electrical signals between cells, enabling the tissue to function as a single unit.
Multi-unit smooth muscle, found in structures like the iris of the eye and the walls of large blood vessels, consists of discrete bundles of cells that are independently innervated.
This arrangement allows for finer, more precise control of contraction, enabling rapid and localized responses.
The functional differences between visceral and multi-unit smooth muscle reflect the diverse physiological roles that smooth muscle plays throughout the body.
Clinical Significance: When Smooth Muscle Goes Wrong
The intricate control smooth muscle exerts throughout the body makes it susceptible to a variety of dysfunctions. When this finely tuned system falters, the consequences can range from mild discomfort to life-threatening conditions. Understanding the clinical implications of smooth muscle dysfunction is crucial for developing effective treatments and improving patient outcomes.
Overview of Smooth Muscle Dysfunction-Related Diseases
Smooth muscle dysfunction manifests in numerous diseases, each impacting specific organ systems. These disorders often arise from abnormalities in the signaling pathways, contractile mechanisms, or regulatory factors that govern smooth muscle activity. The result can be either excessive contraction, insufficient contraction, or uncoordinated activity, leading to a cascade of physiological disruptions.
Examples of Smooth Muscle-Related Diseases
Several common diseases are directly linked to smooth muscle dysfunction. Let’s explore a few key examples:
Asthma: Airway Smooth Muscle in Crisis
Asthma is a chronic respiratory disease characterized by airway inflammation and hyperresponsiveness of airway smooth muscle. Excessive contraction of the bronchial smooth muscle leads to bronchoconstriction, causing difficulty breathing, wheezing, and chest tightness. Inflammatory mediators and allergens trigger this exaggerated response, narrowing the airways and restricting airflow.
Hypertension: Blood Vessel Smooth Muscle Out of Balance
Hypertension, or high blood pressure, is a major risk factor for cardiovascular disease. Dysregulation of smooth muscle in blood vessel walls plays a central role in the development and progression of hypertension. Increased vasoconstriction, due to enhanced smooth muscle contraction or impaired relaxation, elevates peripheral resistance and blood pressure. This sustained elevation can damage blood vessels and increase the risk of heart attack, stroke, and kidney disease.
Irritable Bowel Syndrome (IBS): Intestinal Smooth Muscle in Disarray
Irritable bowel syndrome (IBS) is a common gastrointestinal disorder characterized by abdominal pain, bloating, and altered bowel habits. Abnormal smooth muscle contractions in the intestines contribute significantly to the symptoms of IBS. These contractions can be either too strong, too frequent, or poorly coordinated, leading to pain, diarrhea, or constipation. The exact mechanisms underlying these smooth muscle abnormalities are complex and not fully understood, but factors such as altered gut microbiota, visceral hypersensitivity, and psychological stress are thought to play a role.
Potential Therapeutic Targets
The diverse roles of smooth muscle in various diseases make it an attractive target for therapeutic intervention. Several strategies are being explored to modulate smooth muscle activity and alleviate disease symptoms:
-
Bronchodilators: Medications that relax airway smooth muscle are the mainstay of asthma treatment. Beta-agonists and anticholinergics are commonly used to dilate the airways and improve airflow.
-
Antihypertensive Drugs: Various classes of drugs target smooth muscle in blood vessels to lower blood pressure. Calcium channel blockers, ACE inhibitors, and angiotensin receptor blockers are among the agents used to promote vasodilation and reduce peripheral resistance.
-
Spasmolytics: These medications reduce smooth muscle spasms and contractions in the gastrointestinal tract, providing relief from abdominal pain and cramping associated with conditions like IBS.
-
Targeting Signaling Pathways: Research is ongoing to identify and target specific signaling pathways involved in smooth muscle dysfunction. This includes exploring inhibitors of MLCK, activators of MLCP, and modulators of calcium signaling.
-
Gene Therapy: Gene therapy approaches are being investigated to correct genetic defects that contribute to smooth muscle disorders. This could involve delivering genes that promote smooth muscle relaxation or inhibit excessive contraction.
By understanding the mechanisms underlying smooth muscle dysfunction and developing targeted therapies, we can improve the lives of individuals affected by these debilitating conditions. Further research into smooth muscle physiology and pathology holds great promise for the development of innovative treatments that address the root causes of these diseases.
FAQs: Smooth Muscle Characteristics Explained
Still curious about smooth muscle? Here are some common questions to help clarify its unique features.
How does smooth muscle contraction differ from skeletal muscle contraction?
Smooth muscle contraction is slower and more sustained compared to skeletal muscle. This is due to differences in the mechanisms of calcium regulation and the cycling rate of myosin cross-bridges. Smooth muscle characteristics allow for prolonged contractions without fatigue.
What role does calcium play in smooth muscle contraction?
Calcium is crucial for initiating smooth muscle contraction. It binds to calmodulin, forming a complex that activates myosin light chain kinase (MLCK). MLCK then phosphorylates myosin, enabling it to interact with actin and cause contraction. The concentration of calcium is key in regulating the strength of smooth muscle characteristics.
Where can smooth muscle be found in the body?
Smooth muscle lines the walls of internal organs like the stomach, intestines, bladder, and blood vessels. Its location allows it to control various involuntary functions such as digestion, blood pressure regulation, and bladder emptying. These diverse roles highlight the importance of understanding smooth muscle characteristics.
What are the two main types of smooth muscle and how do they differ?
The two main types are multi-unit and single-unit (or visceral) smooth muscle. Multi-unit smooth muscle consists of discrete, independent cells that are separately stimulated, allowing for fine control. Single-unit smooth muscle cells are connected by gap junctions and contract as a coordinated unit. Different smooth muscle characteristics govern the unique behavior of each type.
So there you have it – your ultimate guide to smooth muscle characteristics! Hopefully, you’ve learned a thing or two. Now go out there and impress your friends with your newfound knowledge! Cheers!