The sliding filament theory provides the foundational mechanism explaining the contraction of sarcomere, a process vital for muscle function. Myosin, a motor protein within the sarcomere, interacts with actin filaments, a process meticulously studied by researchers in labs worldwide and universities for understanding various physiology or disease. The precision of contraction of sarcomere, often analyzed using advanced microscopy techniques is what enables everything from running to breathing.
Muscle contraction, a seemingly simple action, underpins virtually every movement we make, from the most delicate fingertip adjustments to the powerful strides of an athlete. It allows us to breathe, maintain posture, and circulate blood. Understanding the mechanisms behind this fundamental process is critical to grasping human physiology.
At the heart of muscle contraction lies the sarcomere, the basic contractile unit of muscle tissue. This intricate structure, repeated end-to-end along muscle fibers, is where the magic happens.
The Sarcomere: The Engine of Movement
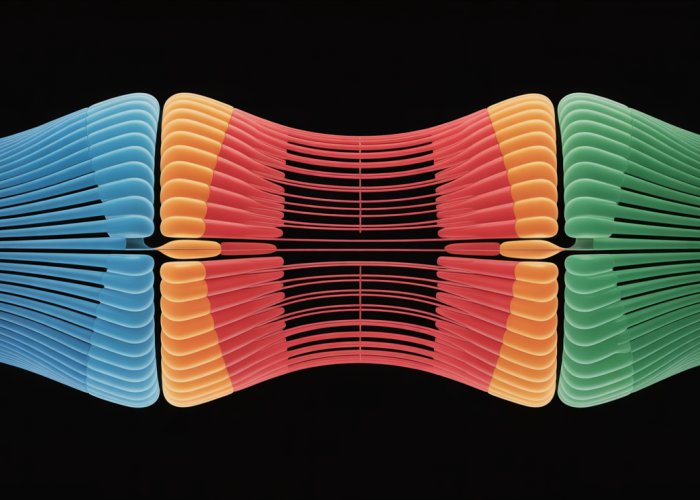
The sarcomere is the fundamental building block responsible for the contraction of striated muscle, the type of muscle that controls voluntary movement and is found in the heart. Defined as the segment between two Z-discs (or Z-lines), it is composed of overlapping protein filaments, primarily actin and myosin.
These filaments interact to slide past each other, shortening the sarcomere and, consequently, the entire muscle fiber. This sliding action is what generates force and produces movement.
Why Sarcomere Contraction Matters
Comprehending sarcomere contraction is not merely an academic exercise. It’s the cornerstone of understanding how our bodies move and function. A deeper knowledge of the sarcomere is essential for:
- Understanding Movement: Sarcomere contraction is the direct mechanism by which our muscles generate force and produce movement. By understanding this process, we can better analyze and optimize human movement.
- Treating Muscle Disorders: Many diseases, such as muscular dystrophies and cardiomyopathies, are rooted in sarcomere dysfunction. A thorough understanding of sarcomere mechanics is crucial for developing effective therapies.
- Enhancing Athletic Performance: Understanding how sarcomeres function allows us to optimize training regimens and potentially enhance athletic performance, maximizing muscle power and efficiency.
- Preventing Injuries: Understanding the limits and vulnerabilities of sarcomere function can help us develop strategies to prevent muscle-related injuries, especially in high-impact activities.
In the following sections, we will delve into the intricate details of the sarcomere, exploring its structure, the molecular mechanisms that drive its contraction, and the factors that regulate its function. Join us as we unlock the secrets of this remarkable biological machine.
The Sarcomere: A Deep Dive into Structure and Components
Understanding the sarcomere’s role in muscle contraction demands a detailed exploration of its anatomical features. This intricate structure, the fundamental unit of muscle contraction, resides within muscle fibers.
Let’s dissect the sarcomere, identifying its key components and their specific functions. From the defining Z-discs to the interacting protein filaments, each element contributes to the remarkable process of muscle contraction.
Defining the Sarcomere and its Location
The sarcomere is the basic functional unit of striated muscle. It’s the repeating unit between two Z-discs. These sarcomeres, linked end-to-end, form myofibrils, which in turn make up muscle fibers.
Within a muscle fiber, sarcomeres are arranged in series, much like train cars connected to form a train. This arrangement allows for the additive effect of shortening, leading to macroscopic muscle contraction.
The Role of the Z-Disc
The Z-disc, or Z-line, acts as the boundary of the sarcomere. It’s a protein structure perpendicular to the muscle fibers, providing an anchoring point for the actin filaments.
Think of the Z-disc as the end of a train car, clearly marking the separation between it and the next. It not only defines the sarcomere’s limits but also helps maintain its structural integrity.
Bands and Zones: Dissecting the Sarcomere’s Appearance
The distinct banding pattern of striated muscle, visible under a microscope, arises from the arrangement of actin and myosin filaments within the sarcomere. These bands and zones provide valuable insights into the sarcomere’s organization:
-
I-band: This light band contains only thin filaments (actin). It spans two adjacent sarcomeres and is bisected by the Z-disc. The I-band shortens during muscle contraction as the actin filaments slide past the myosin filaments.
-
A-band: This dark band runs the entire length of the thick filaments (myosin). It includes the region where actin and myosin overlap and remains constant in length during muscle contraction.
-
H-zone: Located in the middle of the A-band, this region contains only thick filaments (myosin) when the muscle is relaxed. The H-zone narrows during muscle contraction as the actin filaments slide toward the center of the sarcomere, increasing the overlap with myosin.
These bands and zones aren’t just visual markers. They reflect the dynamic interactions of the protein filaments that drive muscle contraction.
Thin Filaments: Actin, Troponin, and Tropomyosin
The thin filaments are primarily composed of the protein actin. Each actin molecule has a binding site for myosin.
However, the interaction between actin and myosin is regulated by two other proteins: troponin and tropomyosin.
-
Tropomyosin: This long, rod-shaped protein wraps around the actin filament, blocking the myosin-binding sites in a relaxed muscle.
-
Troponin: This complex of three proteins (Troponin I, Troponin T, and Troponin C) is bound to both actin and tropomyosin. Troponin plays a critical role in initiating muscle contraction. When calcium ions bind to Troponin C, it triggers a conformational change that moves tropomyosin away from the myosin-binding sites on actin.
Thick Filaments: Myosin
The thick filaments are primarily composed of the protein myosin. Each myosin molecule consists of a long tail and a globular head.
The myosin head contains binding sites for actin and ATP. The heads project outwards from the thick filament, ready to interact with the thin filaments during muscle contraction. It’s the engine that drives filament sliding.
Sliding Filament Theory: The Engine of Muscle Contraction
Having established the intricate architecture of the sarcomere, understanding how it actually contracts is the next logical step. The key lies in the Sliding Filament Theory, the widely accepted mechanism that elucidates muscle contraction at the molecular level.
It explains how the organized arrangement of actin and myosin filaments within the sarcomere translates into the generation of force and the shortening of muscle fibers.
The Foundation of Filament Sliding
At its core, the Sliding Filament Theory posits that muscle contraction occurs due to the sliding of actin (thin) filaments past myosin (thick) filaments.
This sliding action results in the shortening of the sarcomere, and consequently, the entire muscle fiber. It’s crucial to note that neither the actin nor the myosin filaments themselves shorten during this process.
Instead, they maintain their length while sliding across each other, much like extending a telescope.
The Pioneering Work of the Huxleys
The development of the Sliding Filament Theory is attributed to the groundbreaking work of two research teams, most notably Andrew F. Huxley and Hugh E. Huxley (along with Jean Hanson).
Working independently in the 1950s, they provided the evidence that revolutionized our understanding of muscle contraction. Their meticulous observations using electron microscopy revealed that the overlap between actin and myosin filaments increased during muscle contraction, a cornerstone of the theory.
Their work highlighted the dynamic interaction of these proteins, paving the way for future investigations into the molecular mechanisms underlying muscle function.
Actin-Myosin Interaction: The Molecular Dance
The interaction between actin and myosin is the crux of the Sliding Filament Theory. Myosin filaments possess myosin heads (also known as cross-bridges) that bind to specific sites on the actin filaments.
This binding is not constant; it is a cyclical process of attachment, power stroke, detachment, and re-cocking. During the power stroke, the myosin head pivots, pulling the actin filament towards the center of the sarcomere, effectively shortening it.
This action resembles the oars of a boat propelling it forward. The collective action of numerous myosin heads performing these power strokes generates the force required for muscle contraction.
Calcium’s Crucial Role in Initiating Contraction
The interaction between actin and myosin is tightly regulated by calcium ions (Ca2+). In a relaxed muscle, the myosin-binding sites on actin are blocked by tropomyosin, a regulatory protein.
When a nerve impulse reaches the muscle fiber, it triggers the release of calcium ions from the sarcoplasmic reticulum, an internal storage site.
These calcium ions bind to troponin, another regulatory protein associated with actin. This binding causes a conformational change in troponin, which in turn shifts tropomyosin, exposing the myosin-binding sites on actin.
Only then can myosin heads attach to actin and initiate the cross-bridge cycle, leading to muscle contraction. Without calcium, the "brakes" are on, and muscle contraction cannot occur.
ATP: The Energy Currency of Contraction
The entire process of muscle contraction is highly energy-dependent, with ATP (adenosine triphosphate) serving as the primary energy source. ATP plays two critical roles:
- Myosin Head Activation: ATP hydrolysis (the breakdown of ATP into ADP and inorganic phosphate) provides the energy for the myosin head to "cock" into its high-energy conformation, ready to bind to actin.
- Myosin Detachment: ATP binding to the myosin head is essential for its detachment from actin. After the power stroke, ADP is released, but the myosin head remains bound to actin until another ATP molecule binds. This binding weakens the actin-myosin bond, allowing the myosin head to detach and prepare for another cycle.
In the absence of ATP, the myosin head remains bound to actin, resulting in rigor mortis after death. This demonstrates the absolutely essential role of ATP in muscle relaxation as well as contraction.
Having established the crucial roles of actin, myosin, calcium, and ATP in the mechanics of the sarcomere, it becomes imperative to dissect the precise sequence of events that orchestrate muscle contraction. This intricate process is known as the cross-bridge cycle.
The Cross-Bridge Cycle: A Step-by-Step Choreography
The cross-bridge cycle represents the fundamental mechanism by which muscles generate force and contract. It is a recurring sequence of events where myosin heads cyclically bind to actin filaments, pull them inward, detach, and then re-attach further along the actin filament. Each cycle contributes to the sliding of actin past myosin, resulting in sarcomere shortening and ultimately, muscle contraction.
Attachment: Myosin’s Initial Grip on Actin
The cross-bridge cycle begins with the myosin head attaching to the actin filament. This attachment is contingent on the prior availability of binding sites on actin. These sites become accessible following the binding of calcium to troponin and the subsequent repositioning of tropomyosin, which unveils the myosin-binding sites on actin.
The myosin head, now energized by the hydrolysis of ATP from a previous cycle, binds strongly to the newly exposed site on the actin filament. This forms the actin-myosin cross-bridge, the structural foundation for force generation.
The Power Stroke: Generating Force and Filament Sliding
Following the attachment, the myosin head undergoes a conformational change, pivoting and pulling the actin filament towards the center of the sarcomere. This is known as the power stroke.
During the power stroke, the myosin head releases inorganic phosphate (Pi), a product of the ATP hydrolysis that initiated the cycle. This release strengthens the bond between myosin and actin, and provides the energy for the pivotal movement.
As the myosin head pivots, it pulls the actin filament along with it, causing the thin filaments to slide past the thick filaments. This sliding motion shortens the sarcomere, the fundamental event in muscle contraction. ADP is released from the myosin head during the power stroke, but the myosin head remains bound to actin.
Detachment: Breaking the Bond with ATP
For the cross-bridge cycle to continue, the myosin head must detach from the actin filament. This detachment is facilitated by the binding of a new ATP molecule to the myosin head.
The binding of ATP causes a conformational change in the myosin head, weakening its affinity for actin. This weakening allows the myosin head to detach from the actin filament, breaking the cross-bridge.
It’s crucial to note that without ATP, the myosin head remains bound to actin, resulting in a state of rigor. This phenomenon is observed in rigor mortis, the stiffening of muscles after death due to the depletion of ATP.
Re-Cocking: Resetting for the Next Cycle
Once detached, the myosin head is ready to begin another cycle. The newly bound ATP molecule is hydrolyzed into ADP and inorganic phosphate (Pi).
This hydrolysis reaction provides the energy to "re-cock" the myosin head back to its high-energy, extended conformation. The ADP and Pi remain bound to the myosin head, positioning it to bind to another actin molecule further along the filament.
This re-cocking process resets the myosin head, preparing it to form a new cross-bridge and repeat the power stroke. The cycle is now poised to continue as long as calcium is present and ATP is available.
Sustained Contraction: The Repetitive Nature of the Cycle
The cross-bridge cycle is not a one-time event. It repeats continuously as long as the muscle receives signals to contract.
Each cycle contributes to the sliding of actin filaments, and the cumulative effect of numerous cycles leads to significant sarcomere shortening and muscle contraction.
The rate at which the cross-bridge cycle occurs determines the speed of muscle contraction. This rate is influenced by factors such as ATP availability, calcium concentration, and the specific type of muscle fiber involved. This repetitive process, orchestrated by the precise interaction of proteins and energy, is the key to understanding sustained muscular activity.
Having walked through the mechanics of the cross-bridge cycle, the question arises: how is this intricate dance initiated and regulated? The answer lies in the elegant interplay of calcium ions and regulatory proteins that act as the control system for muscle contraction.
Calcium and Regulatory Proteins: The Control System
Muscle contraction isn’t an "always-on" process. It’s carefully regulated to ensure movements are precise and coordinated. Calcium ions (Ca2+), troponin, and tropomyosin are the key players in this regulatory system, dictating when and how muscle fibers contract.
The Regulatory Role of Calcium Ions (Ca2+)
Calcium ions serve as the crucial signal that initiates muscle contraction. In a resting muscle fiber, the concentration of Ca2+ in the sarcoplasm (the cytoplasm of muscle cells) is very low.
When a motor neuron stimulates the muscle fiber, it triggers a cascade of events that ultimately leads to the release of Ca2+ from the sarcoplasmic reticulum, an intracellular storage site.
This sudden surge in Ca2+ concentration is the "go" signal for muscle contraction.
Troponin and Tropomyosin: Gatekeepers of Myosin Binding
Troponin and tropomyosin are proteins intimately associated with the actin filaments. They act as gatekeepers, controlling access to the myosin-binding sites on actin.
Tropomyosin is a long, rod-shaped protein that spirals around the actin filament, physically blocking the myosin-binding sites.
Troponin is a complex of three subunits (Troponin I, Troponin T, and Troponin C) that are attached to tropomyosin.
Together, troponin and tropomyosin form a "blocking complex" that prevents myosin from binding to actin in a resting muscle.
Calcium’s Trigger: Conformational Changes in Troponin
The arrival of calcium ions changes everything. Calcium ions bind to Troponin C, one of the subunits of the troponin complex.
This binding is highly specific and triggers a conformational change in the entire troponin complex.
Think of it like a key fitting into a lock, causing the lock to change shape.
Unmasking Actin: Initiating the Cross-Bridge Cycle
The conformational change in troponin has a direct effect on tropomyosin. The troponin complex, now bound to calcium, pulls tropomyosin away from the myosin-binding sites on actin.
This "unmasking" exposes the binding sites, making them available for myosin heads to attach.
With the myosin-binding sites now accessible, the cross-bridge cycle can begin, leading to muscle contraction. This process is reversible. When calcium levels decrease, calcium detaches from troponin, tropomyosin slides back into its blocking position, and the muscle relaxes.
This intricate regulation ensures that muscle contraction is precisely controlled and responsive to the body’s needs.
Having intricately detailed the roles of calcium and regulatory proteins in initiating muscle contraction, it’s clear that these components act as the signalmen. However, the signal is useless without the fuel to power the action. That fuel, the primary energy currency of the cell, is adenosine triphosphate, or ATP.
ATP: The Fuel for Muscle Power
ATP is not just a fuel for muscle contraction; it is the immediate fuel. This section will explore the multifaceted role of ATP, explaining how it energizes the myosin head, facilitates detachment from actin, and indirectly influences calcium ion regulation. We’ll also briefly touch on alternative energy systems that sustain muscle activity during prolonged exertion.
The Central Role of ATP
ATP’s role extends beyond simple energy provision; it’s integral to multiple stages of the cross-bridge cycle. Without a constant supply of ATP, muscles cannot contract or relax, leading to conditions like rigor mortis, where muscles become locked in a contracted state due to the absence of ATP after death.
ATP Hydrolysis: Powering the Myosin Head
The energy that drives the power stroke comes directly from ATP hydrolysis, the breaking of a phosphate bond in ATP. This process releases energy and converts ATP into adenosine diphosphate (ADP) and inorganic phosphate (Pi).
The myosin head functions as an ATPase enzyme, catalyzing this reaction.
The released energy causes the myosin head to pivot and bind to actin, initiating the power stroke that slides the actin filament toward the center of the sarcomere.
ATP Binding: Facilitating Myosin Detachment
Interestingly, ATP is also required for myosin to detach from actin. After the power stroke, ADP and Pi are released from the myosin head.
A new ATP molecule must then bind to the myosin head, causing it to detach from actin. This detachment is crucial for the cycle to continue, allowing the myosin head to re-cock and bind to a new site on the actin filament.
Without ATP binding, the myosin head remains attached to actin, resulting in a sustained contraction (or, in the absence of any ATP, rigor).
Alternative Energy Sources
While ATP is the immediate fuel, muscles have other mechanisms to regenerate ATP quickly:
-
Creatine Phosphate: This high-energy molecule can rapidly transfer a phosphate group to ADP, regenerating ATP. This system is dominant during short bursts of intense activity, like sprinting or weightlifting.
-
Glycolysis: This anaerobic process breaks down glucose to produce ATP and pyruvate. It’s faster than oxidative phosphorylation but less efficient and produces lactic acid as a byproduct, contributing to muscle fatigue.
-
Oxidative Phosphorylation: This aerobic process, occurring in the mitochondria, uses oxygen to generate ATP from glucose, fatty acids, or amino acids. It’s highly efficient and sustains prolonged muscle activity, such as long-distance running.
These alternative pathways ensure that muscles can continue functioning even when ATP demand outstrips the supply from immediate ATP stores.
Having intricately detailed the roles of calcium and regulatory proteins in initiating muscle contraction, it’s clear that these components act as the signalmen. However, the signal is useless without the fuel to power the action. That fuel, the primary energy currency of the cell, is adenosine triphosphate, or ATP.
From Signal to Contraction: Excitation-Contraction Coupling
Muscle contraction doesn’t begin spontaneously.
It requires a precisely orchestrated chain of events that translates an electrical signal from the nervous system into the mechanical action of sarcomere shortening.
This process, known as excitation-contraction coupling, is the crucial bridge between neural activation and muscle fiber contraction.
The Motor Neuron: The Conductor of Movement
The process begins with a motor neuron, a specialized nerve cell responsible for transmitting signals from the brain or spinal cord to muscle fibers.
Each motor neuron branches out to connect with multiple muscle fibers, forming a motor unit.
When the brain decides to initiate a movement, it sends an electrical impulse down the motor neuron.
This impulse, if strong enough, will eventually trigger the muscle fibers within its motor unit to contract.
The Neuromuscular Junction: Where Nerve Meets Muscle
The site where a motor neuron communicates with a muscle fiber is called the neuromuscular junction.
This is a specialized synapse where the motor neuron’s axon terminal comes into close proximity with the muscle fiber’s membrane, known as the sarcolemma.
However, they don’t physically touch.
Instead, a small gap, the synaptic cleft, separates the two cells.
Events at the Neuromuscular Junction
When the action potential reaches the axon terminal of the motor neuron, it triggers the opening of voltage-gated calcium channels.
Calcium ions (Ca2+) rush into the axon terminal, prompting the fusion of vesicles containing the neurotransmitter acetylcholine (ACh) with the presynaptic membrane.
ACh is then released into the synaptic cleft.
ACh diffuses across the synaptic cleft and binds to acetylcholine receptors (AChRs) located on the sarcolemma of the muscle fiber.
These receptors are ligand-gated ion channels.
When ACh binds, the channels open, allowing sodium ions (Na+) to flow into the muscle fiber and potassium ions (K+) to flow out.
This influx of Na+ depolarizes the sarcolemma, creating a localized depolarization called an end-plate potential (EPP).
Action Potential and Calcium Release: The Trigger for Contraction
If the EPP is large enough to reach a threshold, it initiates an action potential that propagates along the sarcolemma.
The action potential travels down the sarcolemma and into the T-tubules, invaginations of the sarcolemma that penetrate deep into the muscle fiber.
The T-tubules are closely associated with the sarcoplasmic reticulum (SR), an elaborate network of internal membranes that stores calcium ions (Ca2+).
Within the SR membrane are voltage-gated calcium channels called ryanodine receptors.
As the action potential travels down the T-tubules, it activates voltage-sensitive dihydropyridine receptors (DHPRs), which are mechanically coupled to the ryanodine receptors on the SR.
Activation of the DHPRs causes the ryanodine receptors to open, releasing a flood of Ca2+ into the sarcoplasm, the cytoplasm of the muscle fiber.
This sudden increase in sarcoplasmic Ca2+ concentration is the final trigger that initiates the cross-bridge cycle, leading to muscle contraction.
The calcium ions then bind to troponin, initiating the cascade of events that ultimately result in the sliding of actin and myosin filaments and sarcomere shortening, as previously described.
Having intricately detailed the roles of calcium and regulatory proteins in initiating muscle contraction, it’s clear that these components act as the signalmen. However, the signal is useless without the fuel to power the action. That fuel, the primary energy currency of the cell, is adenosine triphosphate, or ATP.
With a firm grasp on the energy source and how it drives the fundamental sliding of filaments, we can now appreciate that this process isn’t a one-size-fits-all affair. Sarcomere contraction, while sharing core principles, manifests uniquely across the different muscle types in our bodies, each adapted to its specific functional demands.
Types of Muscle and Sarcomere Contraction
The elegance of muscle physiology lies in its adaptability. While the sarcomere represents the universal contractile unit, its function is subtly modified to suit the distinct roles of skeletal, cardiac, and smooth muscle.
Understanding these variations is key to appreciating the diverse ways in which our bodies generate force and movement.
Skeletal Muscle: Voluntary Precision
Skeletal muscle, responsible for voluntary movements, is characterized by its highly organized sarcomeres, giving it a striated appearance under a microscope. Its contraction is initiated by nerve impulses, allowing for precise control over force and speed.
Each fiber contracts independently in response to nerve stimulation, which allows for a wide range of movements. Skeletal muscle contraction is typically rapid and forceful, designed for activities ranging from delicate finger movements to powerful weightlifting.
Cardiac Muscle: Involuntary Rhythmicity
Cardiac muscle, found exclusively in the heart, also exhibits striations due to sarcomeric arrangement.
However, its contraction is involuntary and intrinsically rhythmic. Intercalated discs, unique structures connecting adjacent cardiac muscle cells, facilitate rapid spread of electrical signals.
This coordinated electrical activity ensures that the heart contracts as a functional syncytium, pumping blood efficiently throughout the body. Cardiac muscle relies heavily on aerobic metabolism to sustain its continuous activity and is far more resistant to fatigue than skeletal muscle.
Smooth Muscle: Sustained, Involuntary Contractions
Smooth muscle lacks the striated appearance of skeletal and cardiac muscle because its sarcomeres are not as neatly aligned. This type of muscle lines the walls of internal organs, such as the digestive tract and blood vessels, where it carries out slow, sustained, and involuntary contractions.
Instead of troponin, smooth muscle uses calmodulin to initiate contraction, which activates myosin light chain kinase (MLCK), leading to myosin phosphorylation and cross-bridge formation.
Smooth muscle contraction is typically slower and more sustained than skeletal muscle contraction, ideally suited for functions like maintaining blood pressure or propelling food through the digestive system.
Structural Adaptations and Contraction Mechanisms
The structural differences among muscle types directly influence their contraction mechanisms.
Sarcomere Arrangement
-
Skeletal muscle’s well-defined sarcomeres allow for rapid, forceful contractions.
-
Cardiac muscle’s sarcomeres, interconnected by intercalated discs, enable coordinated rhythmic contractions.
-
Smooth muscle’s less organized sarcomeres facilitate slow, sustained contractions.
Regulatory Proteins
-
Skeletal and cardiac muscle utilize troponin and tropomyosin for calcium-mediated regulation of actin-myosin interaction.
-
Smooth muscle relies on calmodulin and MLCK for a different calcium-dependent regulatory pathway.
Innervation
-
Skeletal muscle is innervated by somatic motor neurons, allowing for voluntary control.
-
Cardiac and smooth muscle are innervated by the autonomic nervous system, resulting in involuntary control.
By understanding these structural and functional nuances, we gain a deeper appreciation for the remarkable adaptability of muscle tissue and its crucial role in maintaining overall physiological function. Each muscle type, with its unique sarcomeric architecture and regulatory mechanisms, contributes to the complex symphony of movement and life.
Having intricately detailed the roles of calcium and regulatory proteins in initiating muscle contraction, it’s clear that these components act as the signalmen. However, the signal is useless without the fuel to power the action. That fuel, the primary energy currency of the cell, is adenosine triphosphate, or ATP.
With a firm grasp on the energy source and how it drives the fundamental sliding of filaments, we can now appreciate that this process isn’t a one-size-fits-all affair. Sarcomere contraction, while sharing core principles, manifests uniquely across the different muscle types in our bodies, each adapted to its specific functional demands.
Factors Affecting Sarcomere Contraction
The efficiency and power of sarcomere contraction aren’t solely determined by the intrinsic mechanisms of the sliding filament theory. Several extrinsic and intrinsic factors modulate its strength and speed, influencing overall muscle performance.
These factors dictate how effectively a muscle can generate force, how rapidly it can contract, and how long it can sustain activity before fatigue sets in.
Understanding these modulators is key to comprehending the complexities of muscle physiology and optimizing performance in various contexts.
Muscle Fiber Type: The Foundation of Contractile Capacity
Skeletal muscle isn’t a homogenous tissue; it comprises different fiber types, each with unique contractile and metabolic properties. These variations significantly impact the speed and force of sarcomere contraction.
-
Type I (Slow Oxidative) fibers: These fibers are rich in mitochondria and myoglobin, enabling them to generate ATP primarily through aerobic metabolism. They contract relatively slowly and generate less force but are highly resistant to fatigue, making them ideal for endurance activities.
-
Type IIa (Fast Oxidative-Glycolytic) fibers: These fibers possess characteristics intermediate between Type I and Type IIx. They can utilize both aerobic and anaerobic metabolism, contract faster than Type I fibers, and generate moderate force. They exhibit moderate fatigue resistance.
-
Type IIx (Fast Glycolytic) fibers: These fibers rely heavily on anaerobic glycolysis for ATP production. They contract rapidly and generate substantial force but fatigue quickly due to the rapid accumulation of metabolic byproducts. These are crucial for short bursts of high-intensity activity.
The proportion of each fiber type within a muscle is genetically determined but can be influenced by training. Endurance training can increase the oxidative capacity of muscle fibers, whereas resistance training can promote hypertrophy and increase the proportion of Type II fibers.
Pre-Stretch: Optimizing Sarcomere Length for Peak Performance
The length-tension relationship dictates that the force a muscle can generate is dependent on the initial length of its sarcomeres before contraction. There’s an optimal sarcomere length at which maximal force can be produced.
When a muscle is pre-stretched, the sarcomeres are brought closer to this optimal length.
This pre-stretch increases the number of potential cross-bridge interactions between actin and myosin, leading to a more forceful contraction.
However, excessive stretching can reduce the overlap between filaments, diminishing the number of cross-bridges and reducing force production.
This principle is evident in activities like plyometrics, where a rapid stretch-shortening cycle enhances muscle power output.
Fatigue: The Inevitable Decline in Contractile Function
Muscle fatigue is the decline in muscle force and/or velocity that occurs during sustained or repeated contractions. It’s a complex phenomenon with multiple contributing factors.
-
Energy depletion: Depletion of ATP and other energy substrates can impair cross-bridge cycling and reduce force production.
-
Metabolic byproduct accumulation: Accumulation of lactate, hydrogen ions (H+), and inorganic phosphate can interfere with muscle function by altering pH and inhibiting calcium release and binding.
-
Neuromuscular factors: Fatigue can also arise from impaired signaling at the neuromuscular junction or within the central nervous system.
The specific mechanisms of fatigue vary depending on the intensity and duration of muscle activity. Understanding these mechanisms is critical for developing strategies to delay fatigue and improve athletic performance.
Targeting factors such as buffering capacity, optimizing substrate availability, and improving neuromuscular efficiency can influence the degree to which muscle fatigue affects overall performance.
Having explored the intricate mechanisms driving sarcomere contraction and the factors influencing its efficiency, we now turn our attention to the tangible implications of this knowledge. Understanding the sarcomere isn’t just an academic exercise; it’s a cornerstone for comprehending human health, athletic performance, and the development of treatments for debilitating muscle disorders.
Real-World Applications: Understanding Muscle Function in Health and Disease
The study of sarcomere contraction transcends the laboratory, impacting our comprehension and treatment of various conditions, from genetic diseases to sports-related injuries. A deep understanding of the sarcomere’s function allows us to dissect the underlying causes of muscle dysfunction, paving the way for targeted interventions and improved patient outcomes.
Sarcomere Dysfunction in Muscular Dystrophies
Muscular dystrophies (MD) are a group of genetic diseases characterized by progressive muscle weakness and degeneration. Many forms of MD directly implicate sarcomere dysfunction. Mutations in genes encoding sarcomeric proteins, or proteins that interact with the sarcomere, disrupt the structural integrity and contractile function of muscle fibers.
For example, in Duchenne muscular dystrophy (DMD), a mutation in the dystrophin gene leads to the absence of the dystrophin protein. Dystrophin normally stabilizes the muscle membrane during contraction. Its absence leads to membrane damage, calcium influx, and ultimately, muscle fiber necrosis.
Understanding the precise molecular mechanisms by which these mutations affect sarcomere function is critical for developing effective therapies. Gene therapy, exon skipping, and pharmacological interventions aimed at restoring dystrophin function or mitigating downstream effects are all predicated on a thorough understanding of sarcomere biology.
Sarcomere Mechanics in Sports Performance and Injury Prevention
The efficiency and power of sarcomere contraction are paramount in athletic performance. Athletes rely on the precise orchestration of sarcomere activity to generate force, speed, and endurance. Understanding sarcomere mechanics can inform training strategies, optimize performance, and minimize the risk of injury.
Optimizing Training
Different training modalities elicit specific adaptations in muscle fiber composition and sarcomere structure. Endurance training increases mitochondrial density in muscle fibers, enhancing the capacity for sustained aerobic metabolism and improving fatigue resistance. Resistance training, on the other hand, promotes muscle hypertrophy, increasing the number of sarcomeres within muscle fibers and boosting strength.
Injury Prevention
Eccentric contractions, where the muscle lengthens while contracting, are particularly prone to causing muscle damage. A detailed knowledge of sarcomere mechanics allows athletes and trainers to design training programs that strengthen muscles in eccentric phases, minimizing the risk of strains and tears. Furthermore, understanding the role of proper warm-up and stretching in preparing the sarcomere for activity is crucial for preventing injuries.
Therapeutic Development for Muscle-Related Disorders
A comprehensive understanding of sarcomere function is essential for developing targeted therapies for a wide range of muscle-related disorders, not just muscular dystrophies. This includes conditions such as heart failure (where sarcomere dysfunction impairs cardiac contractility) and sarcopenia (age-related muscle loss).
Pharmaceutical Interventions
Many drugs target specific aspects of sarcomere function. For example, some drugs aim to improve calcium sensitivity in heart failure patients, enhancing the force of cardiac contraction. Others focus on inhibiting pathways that lead to muscle atrophy in conditions like cancer cachexia.
Gene and Cell Therapies
Gene therapy holds promise for correcting genetic defects that directly impact sarcomere structure and function. Cell-based therapies, involving the transplantation of healthy muscle cells, may offer a means of replacing damaged muscle tissue in patients with severe muscle loss. All these approaches are rooted in a fundamental understanding of sarcomere biology and the mechanisms that govern muscle contraction.
Sarcomere Contraction: Frequently Asked Questions
[This FAQ section addresses common questions about sarcomere contraction to further clarify the concepts discussed in the ultimate guide.]
What exactly triggers the contraction of a sarcomere?
The contraction of a sarcomere is initiated by the release of calcium ions (Ca2+) from the sarcoplasmic reticulum. These calcium ions bind to troponin, causing a conformational change that exposes the myosin-binding sites on actin filaments.
How does ATP contribute to sarcomere contraction?
ATP is essential for the myosin head to detach from the actin filament after the power stroke. Without ATP, the myosin head remains bound, resulting in rigor mortis. ATP hydrolysis also provides the energy for the myosin head to re-cock and prepare for the next contraction cycle.
What happens to the H zone and I band during sarcomere contraction?
During the contraction of a sarcomere, the H zone (containing only myosin) and the I band (containing only actin) shorten. This occurs as the actin filaments slide past the myosin filaments, bringing the Z discs closer together.
Is sarcomere contraction an all-or-nothing process?
While a single sarcomere contraction is triggered by an action potential, the overall strength of muscle contraction is not all-or-nothing. It depends on the number of motor units activated and the frequency of stimulation. This allows for varying degrees of force generation.
So, next time you’re crushing that workout or even just grabbing a coffee, remember the incredible process of contraction of sarcomere happening within your muscles! Hopefully, you now have a better understanding of how it all works.