The sarcolemma, analogous to the plasma membrane in other cells, plays a critical role in muscle fiber function. Actin and Myosin filaments, essential components of muscle contraction, are directly impacted by the sarcolemma’s integrity and function. Understanding the function of sarcolemma is paramount for researchers at institutions like the National Institutes of Health (NIH) studying muscular diseases, as its unique structure facilitates the transmission of action potentials and maintains cellular homeostasis vital for muscular activity. The sarcolemma’s intricate relationship with the sarcoplasmic reticulum further underscores its importance in regulating calcium ion concentration, a key factor in triggering muscle contraction and relaxation.
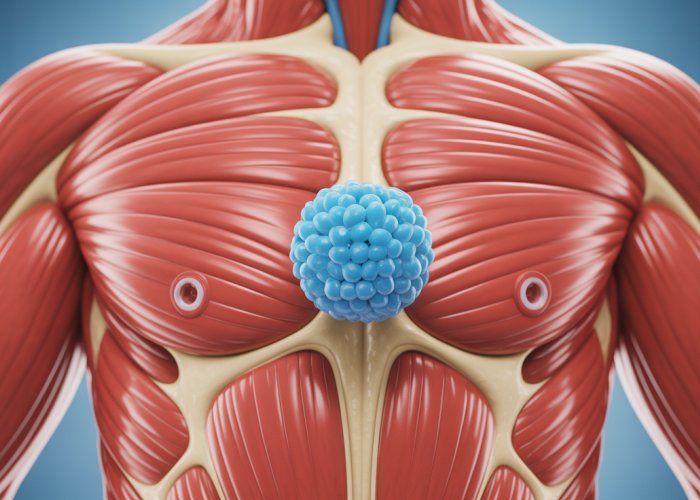
The human body is a marvel of intricate systems, and at the heart of movement lies the muscle fiber. Encasing each of these fibers is a specialized cell membrane known as the sarcolemma. This isn’t just a passive barrier; it’s a dynamic interface, a gatekeeper controlling the flow of information and materials that dictate muscle function.
Defining the Sarcolemma
The sarcolemma is the cell membrane of a muscle fiber, a thin, selectively permeable membrane that surrounds the muscle cell. It’s located directly beneath the endomysium, a connective tissue layer that surrounds individual muscle fibers.
Imagine it as the "skin" of the muscle cell, but far more complex than simple protective wrapping.
The sarcolemma isn’t just a barrier; it’s a dynamic interface, controlling what enters and exits the muscle cell.
The Sarcolemma: A Key to Muscle Physiology
Understanding the sarcolemma’s function is paramount to grasping the complexities of muscle physiology. It’s the site where signals from the nervous system are received, processed, and translated into the mechanical work of muscle contraction.
Its integrity and proper function are crucial not only for athletic performance but also for maintaining overall muscle health and preventing debilitating diseases.
Without a properly functioning sarcolemma, muscles cannot contract efficiently, leading to weakness, fatigue, and potentially severe health consequences.
Thesis: The Sarcolemma as the Interface Between Nerve and Muscle
The sarcolemma is essential for muscle excitation, contraction, and overall muscle function. It acts as the primary interface between the nervous system and the muscle cell, orchestrating the intricate dance of electrical and chemical signals that drive movement.
It’s the critical link in the chain of events that allows us to walk, run, lift, and perform countless other physical activities. Delving into its structure and function unlocks a deeper appreciation for the elegance and efficiency of human movement.
The human body is a marvel of intricate systems, and at the heart of movement lies the muscle fiber. Encasing each of these fibers is a specialized cell membrane known as the sarcolemma. This isn’t just a passive barrier; it’s a dynamic interface, a gatekeeper controlling the flow of information and materials that dictate muscle function. Now that we’ve established the sarcolemma’s vital role as the interface between nerve and muscle, it’s time to examine its structure. This will reveal how its specialized design enables it to carry out its crucial functions.
Sarcolemma Structure: A Specialized Cell Membrane
The sarcolemma is more than just a simple covering; it’s a highly specialized structure. It has unique features that differentiate it from typical cell membranes. Understanding its components is key to understanding how it orchestrates muscle excitation and contraction.
The Foundation: Lipid Bilayer and Membrane Proteins
At its core, the sarcolemma shares the fundamental structure of all cell membranes: a phospholipid bilayer.
This barrier is composed of two layers of phospholipid molecules. Hydrophilic heads face outward towards the watery environments inside and outside the cell. Hydrophobic tails face inward, creating a barrier to water-soluble substances.
Embedded within this lipid bilayer are a variety of proteins, each with specialized functions.
These proteins serve as channels, receptors, enzymes, and structural components, contributing to the sarcolemma’s dynamic nature.
Unique Features of the Sarcolemma
While the basic lipid bilayer structure is consistent, the sarcolemma possesses distinct features tailored to its role in muscle physiology.
These include a high concentration of receptors, specialized ion channels, and the presence of T-tubules, all of which contribute to its unique functionality.
Receptors: Receiving Signals
The sarcolemma is studded with receptors that bind to signaling molecules, most notably acetylcholine.
These receptors are concentrated at the neuromuscular junction, the point of contact between a motor neuron and the muscle fiber.
When acetylcholine binds to these receptors, it triggers a cascade of events that ultimately lead to muscle contraction.
Ion Channels: Controlling the Flow
Ion channels are transmembrane proteins that allow specific ions to pass through the sarcolemma.
These channels are crucial for generating and propagating the action potential, the electrical signal that travels along the muscle fiber and initiates contraction.
Voltage-gated sodium channels, potassium channels, and calcium channels are particularly important for muscle function.
T-Tubules: Extending the Sarcolemma
T-tubules (transverse tubules) are unique invaginations of the sarcolemma. They penetrate deep into the muscle fiber, forming a network of tunnels.
This network ensures that the action potential can rapidly reach all parts of the muscle fiber, triggering a uniform contraction.
The T-tubules are closely associated with the sarcoplasmic reticulum, a network of intracellular membranes that store calcium ions.
Structure Dictates Function: Facilitating Excitation and Contraction
The specialized structures of the sarcolemma are not merely decorative; they are essential for muscle excitation and contraction.
The receptors at the neuromuscular junction allow the muscle fiber to receive signals from the nervous system.
The ion channels enable the generation and propagation of the action potential.
The T-tubules ensure that the signal reaches all parts of the muscle fiber quickly and efficiently.
Together, these features enable the sarcolemma to act as the critical interface between nerve and muscle, orchestrating the complex process of muscle contraction. Without this specialized structure, muscles would be unable to respond to nervous stimulation and generate movement.
Initiating Contraction: The Neuromuscular Junction and Sarcolemma’s Role
Having explored the specialized structure of the sarcolemma, we now turn our attention to its crucial role in initiating muscle contraction. This process begins at the neuromuscular junction (NMJ), the vital communication point between a motor neuron and the muscle fiber. It is at this specialized synapse where the nervous system communicates directly with the muscle, setting the stage for the complex sequence of events that ultimately leads to movement.
The Neuromuscular Junction: Where Nerve Meets Muscle
The neuromuscular junction is not a physical connection, but rather a specialized synapse.
It’s a highly organized structure that ensures efficient and reliable transmission of signals from the motor neuron to the muscle fiber.
Effectively, it’s the command center for muscle activation.
The NMJ comprises several key components: the motor neuron terminal, the synaptic cleft, and the motor end plate on the sarcolemma.
-
Motor Neuron Terminal: This is the endpoint of the motor neuron, containing vesicles filled with the neurotransmitter acetylcholine (ACh).
-
Synaptic Cleft: This is the narrow gap (20-40 nm) separating the motor neuron terminal and the sarcolemma. Neurotransmitters must diffuse across this space to transmit the signal.
-
Motor End Plate: This is a specialized region of the sarcolemma that is highly folded to increase surface area. It’s densely populated with acetylcholine receptors (AChRs).
These receptors are ligand-gated ion channels that open upon binding of ACh, allowing ions to flow across the membrane.
Acetylcholine Release and Receptor Binding
The process of initiating muscle contraction begins with a signal from the central nervous system that travels down the motor neuron.
When the action potential reaches the motor neuron terminal, it triggers an influx of calcium ions (Ca2+) into the terminal.
This influx of Ca2+ is essential for the next step: the release of acetylcholine (ACh).
Ca2+ entry causes the synaptic vesicles containing ACh to fuse with the presynaptic membrane of the motor neuron terminal.
This fusion results in exocytosis, the process by which ACh is released into the synaptic cleft.
Once released, ACh diffuses rapidly across the synaptic cleft to reach the motor end plate on the sarcolemma.
Here, ACh binds to its specific receptors (AChRs).
The AChRs are strategically located on the folds of the motor end plate to maximize the likelihood of binding.
The binding of ACh to AChRs is a crucial step, acting as the trigger that initiates downstream events in the muscle fiber.
Depolarization of the Sarcolemma: A Cascade of Events
The binding of acetylcholine (ACh) to its receptors (AChRs) on the sarcolemma doesn’t directly cause muscle contraction.
Instead, it initiates a change in the sarcolemma’s permeability to ions, specifically sodium (Na+) and potassium (K+).
AChRs are ligand-gated ion channels, meaning they open in response to the binding of a specific chemical messenger (in this case, ACh).
When ACh binds, the AChRs open, allowing Na+ ions to flow into the muscle fiber and K+ ions to flow out, but predominantly allowing Na+ to flow into the cell.
The influx of positively charged Na+ ions into the muscle fiber causes the inside of the sarcolemma to become less negative, moving it towards a more positive charge.
This change in membrane potential is known as depolarization.
If the depolarization reaches a certain threshold, it triggers the opening of voltage-gated sodium channels in the sarcolemma surrounding the motor end plate.
This further influx of Na+ ions causes a rapid and substantial depolarization of the sarcolemma, generating an action potential.
This action potential then propagates along the sarcolemma, ultimately leading to muscle contraction, as we’ll explore in subsequent sections.
Having established the crucial role of acetylcholine in initiating muscle contraction at the neuromuscular junction, we now delve deeper into the sarcolemma’s response to this initial stimulus. The binding of acetylcholine triggers a cascade of electrical events across the sarcolemma, ultimately leading to the generation and propagation of an action potential – the very signal that drives muscle contraction.
Action Potential: The Electrical Signal Across the Sarcolemma
The action potential is a rapid, transient change in the electrical potential across the sarcolemma, the muscle fiber’s cell membrane. It’s essentially a wave of depolarization that sweeps along the sarcolemma’s surface, carrying the signal for muscle contraction from the neuromuscular junction to the depths of the muscle fiber.
This electrical signal is not merely a side effect; it’s the essential trigger for the events that lead to the interaction of actin and myosin filaments, the molecular basis of muscle contraction.
The Significance of the Action Potential
The action potential is significant because it provides a rapid, reliable, and long-distance communication system within the muscle fiber.
It ensures that the signal to contract is delivered quickly and uniformly to all parts of the muscle fiber, allowing for coordinated and powerful contractions.
Without the action potential, the initial stimulus at the neuromuscular junction would remain localized, and only a small portion of the muscle fiber would contract.
Phases of the Action Potential: A Precise Sequence of Events
The action potential unfolds in a highly orchestrated sequence of phases, each characterized by specific changes in the sarcolemma’s permeability to ions. These phases are:
-
Polarization (Resting Membrane Potential): In its resting state, the sarcolemma maintains a negative electrical potential inside the cell relative to the outside. This is known as the resting membrane potential, typically around -70 to -90 millivolts (mV).
This polarized state is crucial for the muscle fiber to be ready to respond to a stimulus. It’s maintained by the unequal distribution of ions, primarily sodium (Na+) and potassium (K+), across the sarcolemma.
-
Depolarization: When acetylcholine binds to its receptors at the motor end plate, it triggers the opening of ligand-gated ion channels. This allows an influx of sodium ions (Na+) into the muscle fiber.
The influx of positively charged sodium ions causes the inside of the sarcolemma to become less negative, moving towards a more positive potential.
If the depolarization reaches a threshold level (around -55 mV), it triggers the opening of voltage-gated sodium channels.
These channels allow a rapid and massive influx of sodium, causing the membrane potential to rapidly spike to a positive value (around +30 mV). This rapid change is the depolarization phase of the action potential. -
Repolarization: After a brief period of depolarization, the voltage-gated sodium channels quickly inactivate, halting the influx of sodium ions.
Simultaneously, voltage-gated potassium channels open, allowing potassium ions (K+) to flow out of the muscle fiber.
The outflow of positively charged potassium ions restores the negative electrical potential inside the sarcolemma, bringing it back towards the resting membrane potential.
This return to a negative potential is the repolarization phase. -
Hyperpolarization (Optional): In some cases, the repolarization phase can overshoot the resting membrane potential, resulting in a brief period of hyperpolarization.
This occurs because the potassium channels remain open for a short time after the membrane potential has returned to its resting level.
The hyperpolarization phase ensures that the action potential is a discrete event and prevents the muscle fiber from being continuously stimulated.
The Roles of Sodium and Potassium Ions
The action potential is fundamentally driven by the movement of sodium (Na+) and potassium (K+) ions across the sarcolemma.
These ions are not simply passive participants; they are the key players in the electrical events that underlie muscle contraction.
-
Sodium Ions (Na+): Sodium ions are primarily responsible for the depolarization phase of the action potential. Their influx into the muscle fiber causes the rapid reversal of the membrane potential, triggering the electrical signal that travels along the sarcolemma.
-
Potassium Ions (K+): Potassium ions are primarily responsible for the repolarization phase of the action potential. Their outflow from the muscle fiber restores the negative membrane potential, allowing the muscle fiber to reset and prepare for the next stimulus.
The precise control of sodium and potassium ion movement is achieved through specialized ion channels embedded within the sarcolemma. These channels are selectively permeable to specific ions and are regulated by voltage or ligands, ensuring the proper timing and amplitude of the action potential.
Propagation Along the Sarcolemma and into the T-Tubules
The action potential doesn’t just occur at a single point on the sarcolemma; it propagates along the entire length of the muscle fiber.
This propagation is crucial for ensuring that all parts of the muscle fiber are stimulated to contract simultaneously.
As the depolarization wave spreads along the sarcolemma, it triggers the opening of voltage-gated sodium channels in adjacent regions of the membrane, causing the action potential to propagate forward like a chain reaction.
Importantly, the action potential also travels down the T-tubules, which are invaginations of the sarcolemma that extend deep into the muscle fiber. This is crucial because it allows the electrical signal to reach the sarcoplasmic reticulum, the intracellular calcium store, which is essential for initiating muscle contraction.
Having established the crucial role of acetylcholine in initiating muscle contraction at the neuromuscular junction, we now delve deeper into the sarcolemma’s response to this initial stimulus. The binding of acetylcholine triggers a cascade of electrical events across the sarcolemma, ultimately leading to the generation and propagation of an action potential – the very signal that drives muscle contraction.
T-Tubules: Extending the Signal Deep Within the Muscle Fiber
While the action potential rapidly propagates across the sarcolemma’s surface, the muscle fiber’s considerable size presents a challenge. How does this electrical signal reach the myofibrils, the contractile units deep within the cell, to trigger a coordinated contraction? The answer lies in a remarkable network of invaginations called T-tubules, or transverse tubules.
The Architecture of T-Tubules: A Deep Dive
Imagine the sarcolemma, not as a simple, smooth membrane, but as one intricately folded inwards at regular intervals. These inward folds form the T-tubules, essentially creating a network of tunnels that plunge deep into the sarcoplasm, the muscle fiber’s cytoplasm.
These tubules are not isolated structures; they are continuous with the extracellular space, meaning the fluid within the T-tubules has a similar ionic composition to the fluid surrounding the muscle fiber. This continuity is crucial for the rapid transmission of the action potential.
The strategic location of T-tubules is also critical. They are positioned close to the sarcoplasmic reticulum (SR), a specialized endoplasmic reticulum that stores calcium ions, the ultimate trigger for muscle contraction. This close proximity forms what is known as a triad: a T-tubule flanked by two terminal cisternae of the SR.
Rapid and Uniform Signal Transmission
The primary function of T-tubules is to ensure the rapid and uniform transmission of the action potential to all parts of the muscle fiber. Without them, the action potential would remain confined to the sarcolemma’s surface, and the contraction would be slow and uneven, affecting only the superficial myofibrils.
Because the T-tubules are continuous with the sarcolemma, the action potential propagates along their membranes, penetrating deep into the muscle fiber. This allows the signal to reach the myofibrils almost simultaneously, triggering a coordinated and powerful contraction.
Consider the analogy of a city’s transportation system. The sarcolemma is like the main highway, carrying the initial wave of traffic (the action potential). The T-tubules are like the branching side streets and subway lines, ensuring that the traffic (the signal) reaches every neighborhood (myofibril) quickly and efficiently.
The T-Tubule-Sarcoplasmic Reticulum Connection: A Crucial Partnership
The close relationship between T-tubules and the sarcoplasmic reticulum (SR) is fundamental to excitation-contraction coupling, the process by which the electrical signal of the action potential is converted into a mechanical contraction.
As the action potential travels down the T-tubule, it activates voltage-sensitive proteins called dihydropyridine receptors (DHPRs), which are located on the T-tubule membrane. These DHPRs are mechanically linked to ryanodine receptors (RyRs) on the SR membrane.
When the DHPRs detect the voltage change associated with the action potential, they undergo a conformational change, which directly or indirectly opens the RyRs. This, in turn, allows calcium ions to flood out of the SR and into the sarcoplasm, initiating the cascade of events that lead to muscle contraction.
The T-tubules, therefore, are not merely passive conduits; they play an active role in triggering the release of calcium ions from the SR, bridging the gap between the electrical signal and the mechanical response. Their strategic location and intimate connection with the SR make them indispensable for efficient and coordinated muscle function.
Having navigated the intricate network of T-tubules that channel the action potential deep within the muscle fiber, the stage is now set for the pivotal event that directly initiates muscle contraction: the release of calcium ions. This carefully orchestrated release, emanating from the sarcoplasmic reticulum, transforms the electrical signal into a chemical one, bridging the gap between excitation and the mechanical process of muscle fiber shortening.
Calcium Release: The Trigger for Muscle Contraction
The action potential, having journeyed along the sarcolemma and plunged into the depths via the T-tubules, arrives at its ultimate destination: the sarcoplasmic reticulum (SR). This specialized organelle, a modified form of the endoplasmic reticulum, acts as the primary calcium reservoir within the muscle fiber. Understanding its structure and function is critical to appreciating how calcium release is triggered and regulated.
The Sarcoplasmic Reticulum: A Calcium Reservoir
The sarcoplasmic reticulum is an elaborate network of interconnected tubules that surround each myofibril, the contractile unit of the muscle fiber. Its primary function is to sequester and store calcium ions (Ca2+), maintaining a significantly higher concentration of calcium within its lumen compared to the surrounding sarcoplasm (cytoplasm of the muscle cell).
This concentration gradient is maintained by ATP-dependent calcium pumps (SERCA – Sarcoplasmic/Endoplasmic Reticulum Calcium ATPase) embedded in the SR membrane. These pumps actively transport calcium ions from the sarcoplasm into the SR lumen, ensuring that the intracellular calcium concentration remains low at rest, preventing unwanted muscle contraction.
The Action Potential’s Role in Calcium Release
The arrival of the action potential at the T-tubules initiates a cascade of events that culminates in the opening of calcium channels on the SR membrane. This process involves a crucial interaction between two key protein receptors: dihydropyridine receptors (DHPRs) located on the T-tubule membrane and ryanodine receptors (RyRs) situated on the SR membrane.
DHPR and RyR Interaction: A Lock-and-Key Mechanism
Dihydropyridine receptors (DHPRs) are voltage-sensitive calcium channels located on the T-tubule membrane. Upon depolarization of the T-tubule membrane by the action potential, DHPRs undergo a conformational change.
This conformational change acts as a mechanical trigger, directly interacting with ryanodine receptors (RyRs) on the SR membrane. RyRs are calcium release channels, and their activation leads to a rapid efflux of calcium ions from the SR lumen into the sarcoplasm.
In skeletal muscle, the DHPR and RyR are physically coupled, meaning the conformational change in DHPR directly opens the RyR channel. In cardiac muscle, the mechanism is slightly different: calcium influx through DHPRs triggers the opening of RyRs, a process known as calcium-induced calcium release (CICR).
The Floodgates Open: Calcium’s Journey to the Myofibrils
The release of calcium ions from the SR dramatically increases the calcium concentration in the sarcoplasm surrounding the myofibrils. This surge of calcium is the critical trigger for muscle contraction.
These calcium ions then bind to troponin, a protein complex associated with actin filaments, initiating a series of events that ultimately allow myosin to bind to actin and initiate the sliding filament mechanism, the fundamental process underlying muscle contraction. Without this precisely controlled release of calcium, the muscle would remain at rest, unable to respond to neural stimulation.
Having orchestrated the crucial release of calcium, the spotlight now shifts to the sarcolemma’s enduring role in the entire contraction cycle. It’s not merely a trigger, but a constant guardian of the cellular environment that allows muscle fibers to contract and relax efficiently. The sarcolemma, along with its associated structures, works in concert to ensure that the muscle fiber is always ready to respond to the next signal.
Sarcolemma’s Role in the Contraction Cycle: Maintaining Membrane Potential
The sarcolemma’s contribution to muscle contraction extends far beyond the initial action potential. It is fundamentally responsible for maintaining the resting membrane potential, the electrical foundation upon which all muscle activity is built. Without this carefully established and maintained potential, the muscle fiber would be unable to generate action potentials, and contraction would be impossible.
The Resting Membrane Potential: A Foundation for Excitability
The resting membrane potential is established by an unequal distribution of ions across the sarcolemma. This is primarily driven by the sodium-potassium pump (Na+/K+ ATPase), which actively transports sodium ions (Na+) out of the cell and potassium ions (K+) into the cell.
Leak channels, which are selectively permeable to either Na+ or K+, also play a vital role. More K+ leak channels than Na+ leak channels exist, making the membrane more permeable to potassium. This leads to a net efflux of K+ ions, creating a negative charge inside the cell relative to the outside.
This charge difference, typically around -70 to -90 mV in muscle cells, is the resting membrane potential. It represents stored potential energy, ready to be unleashed when the muscle fiber is stimulated.
Orchestrating Contraction: A Symphony of Structures and Ions
The sarcolemma, T-tubules, and sarcoplasmic reticulum (SR) function as an integrated system to facilitate muscle contraction.
Here’s how they coordinate to bring about the sliding filament mechanism:
-
Action Potential Arrival: The process begins with an action potential propagating along the sarcolemma and into the T-tubules.
-
Calcium Release: The T-tubules, acting as conduits, transmit the signal deep into the muscle fiber, triggering the release of calcium ions (Ca2+) from the SR.
-
Calcium Binding and Myofilament Interaction: The released calcium ions bind to troponin, a protein on the thin filaments (actin). This binding causes a conformational change in tropomyosin, exposing the myosin-binding sites on actin.
-
Cross-Bridge Cycling: Myosin heads can now bind to actin, forming cross-bridges. ATP hydrolysis provides the energy for the myosin heads to pull the actin filaments towards the center of the sarcomere, shortening the muscle fiber.
-
Relaxation: To initiate relaxation, the action potential ceases. The SR actively pumps calcium ions back into its lumen, reducing the calcium concentration in the sarcoplasm.
This causes calcium to detach from troponin, allowing tropomyosin to cover the myosin-binding sites on actin once again. Cross-bridge cycling stops, and the muscle fiber relaxes.
The sarcolemma’s role extends beyond just initiating this process. It’s also vital in maintaining the ion gradients necessary for repeated cycles of excitation and contraction.
Sarcolemma Variations Across Muscle Types
While the fundamental principles of sarcolemma function are similar across different muscle types (skeletal, cardiac, and smooth), there are notable differences that reflect their distinct contractile properties and regulatory mechanisms.
-
Skeletal Muscle: Skeletal muscle sarcolemma possesses well-defined T-tubules and a highly organized SR for rapid and powerful contractions. Its excitation-contraction coupling is primarily controlled by the nervous system.
-
Cardiac Muscle: Cardiac muscle sarcolemma has T-tubules that are wider and less numerous than those in skeletal muscle. Cardiac muscle relies on calcium-induced calcium release (CICR), where a small influx of extracellular calcium triggers the release of a larger amount of calcium from the SR. Intercalated discs, specialized junctions between cardiac muscle cells, allow for rapid electrical communication.
-
Smooth Muscle: Smooth muscle sarcolemma lacks T-tubules, and its SR is less developed than in skeletal or cardiac muscle. Contraction is regulated by various factors, including hormonal signals and local tissue conditions. Calcium entry from the extracellular space plays a more significant role in smooth muscle contraction than in skeletal muscle.
Having orchestrated the crucial release of calcium, the spotlight now shifts to the sarcolemma’s enduring role in the entire contraction cycle. It’s not merely a trigger, but a constant guardian of the cellular environment that allows muscle fibers to contract and relax efficiently. The sarcolemma, along with its associated structures, works in concert to ensure that the muscle fiber is always ready to respond to the next signal.
Clinical Relevance: When the Sarcolemma Fails
The intricate functions of the sarcolemma, from maintaining membrane potential to propagating action potentials, are critical for proper muscle function. When this delicate system is disrupted, the consequences can manifest as a range of debilitating conditions. Understanding these conditions highlights the sarcolemma’s profound impact on overall health, movement, and quality of life.
Muscular Dystrophies: A Structural Breakdown
Muscular dystrophies represent a group of genetic disorders characterized by progressive muscle weakness and degeneration. Many of these conditions directly involve defects in proteins associated with the sarcolemma, compromising its structural integrity and functional capacity.
Duchenne muscular dystrophy (DMD), for example, arises from mutations in the dystrophin gene. Dystrophin is a crucial protein that links the sarcolemma to the internal cytoskeleton of the muscle fiber, providing stability during contraction.
Without functional dystrophin, the sarcolemma becomes fragile and susceptible to damage, leading to muscle fiber breakdown and eventual replacement with connective tissue. This results in progressive weakness, impacting mobility, respiratory function, and cardiac health.
Other muscular dystrophies, such as limb-girdle muscular dystrophies (LGMDs), can also involve defects in sarcolemma-associated proteins, leading to similar, though sometimes less severe, muscle degeneration. The specific proteins affected and the patterns of muscle involvement vary depending on the type of LGMD.
Ion Channelopathies: Disrupting Electrical Excitability
The sarcolemma’s ability to generate and propagate action potentials depends on the precise function of ion channels, specialized proteins that regulate the flow of ions across the membrane. Ion channelopathies are a group of disorders caused by mutations in genes encoding these ion channels, disrupting the electrical excitability of muscle fibers.
Myotonia, a hallmark of several ion channelopathies, is characterized by delayed muscle relaxation after voluntary contraction. This occurs due to prolonged depolarization of the sarcolemma, often resulting from defects in chloride channels (e.g., in myotonia congenita) or sodium channels (e.g., in paramyotonia congenita).
Periodic paralysis is another manifestation of ion channelopathies, characterized by episodes of muscle weakness or paralysis. These episodes can be triggered by changes in serum potassium levels and are often associated with mutations in sodium or calcium channels.
These conditions highlight the critical role of ion channels in maintaining the sarcolemma’s electrical properties and ensuring proper muscle function. Disruptions in ion channel activity can lead to significant impairments in muscle contraction and relaxation.
The Broader Impact: Health, Movement, and Performance
The sarcolemma’s integrity is not only essential for muscle function but also for overall health, movement, and physical performance. When the sarcolemma is compromised, even seemingly minor activities can become challenging.
Maintaining balance, walking, and performing everyday tasks require the coordinated contraction and relaxation of various muscle groups, all dependent on proper sarcolemma function.
Athletes, in particular, rely on the sarcolemma’s ability to rapidly and efficiently transmit signals for optimal muscle performance. Defects in sarcolemma function can impair strength, speed, and endurance, limiting athletic potential.
Furthermore, the sarcolemma’s role extends beyond skeletal muscle. Cardiac muscle and smooth muscle also rely on proper sarcolemma function for heart function, vascular tone, and gastrointestinal motility.
Disruptions in sarcolemma function in these tissues can lead to a range of serious health problems.
In conclusion, the clinical relevance of the sarcolemma cannot be overstated. Its proper function is essential for maintaining muscle health, enabling movement, and supporting overall physiological well-being. Understanding the diseases and conditions that affect the sarcolemma is crucial for developing effective diagnostic and therapeutic strategies to improve the lives of individuals affected by these disorders.
Sarcolemma FAQs: Unveiling Its Vital Role
This FAQ section addresses common questions regarding the sarcolemma and its importance in muscle function. We aim to clarify its role and significance for better understanding.
What exactly is the sarcolemma?
The sarcolemma is the plasma membrane that surrounds each muscle fiber. Think of it as the cell membrane for muscle cells. This critical structure is responsible for maintaining the integrity of the cell and its ionic environment.
How does the function of sarcolemma relate to muscle contraction?
The sarcolemma plays a crucial role in propagating action potentials, the electrical signals that trigger muscle contraction. It contains ion channels and receptors that allow these signals to travel across the muscle fiber, initiating the contractile process. Without proper sarcolemma function, muscles wouldn’t be able to contract.
What happens if the sarcolemma is damaged?
Damage to the sarcolemma can disrupt its ability to conduct action potentials and maintain cellular integrity. This can lead to muscle weakness, atrophy, and even cell death. Various muscular dystrophies are related to issues affecting the sarcolemma and its associated proteins.
Where are the T-tubules located, and what do they do?
T-tubules, or transverse tubules, are invaginations of the sarcolemma that extend deep into the muscle fiber. These tubules bring the action potential closer to the sarcoplasmic reticulum, which stores calcium ions. This proximity ensures rapid and uniform muscle contraction as it facilitates calcium release. They work intimately with the function of sarcolemma to ensure the electrical signal reaches all parts of the cell.
So, that’s a wrap on the function of sarcolemma! Hopefully, you’ve got a clearer picture of how this essential part of your muscle cells works. Now, go flex those muscles, and remember to thank your sarcolemma!