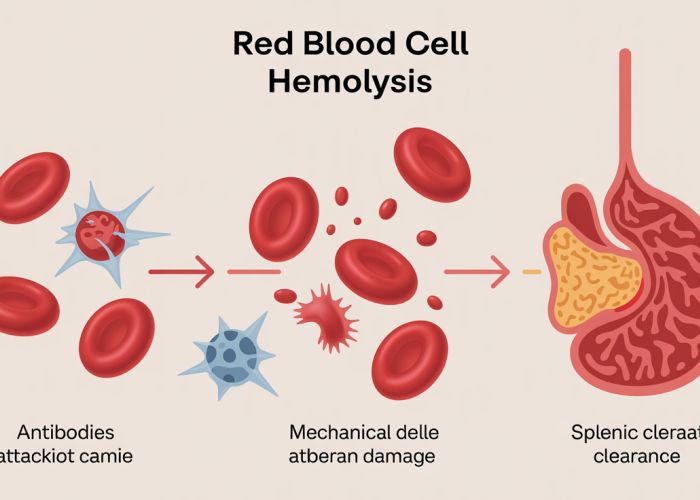
Hemolysis, a critical process in the human body, is significantly impacted by rbc destruction causes. Understanding these causes is vital, as conditions like autoimmune hemolytic anemia, often diagnosed through techniques leveraging flow cytometry, can result in excessive erythrocyte breakdown. This breakdown subsequently affects organs such as the spleen, which filters and removes damaged red blood cells, showcasing the interconnectedness of body systems affected by rbc destruction causes.
Understanding RBC Destruction Causes: A Comprehensive Layout Guide
An effective article addressing "RBC destruction causes" needs to be informative, logically structured, and easily digestible for the reader. This outline focuses on clarity and providing a comprehensive overview of the topic.
Introduction: Setting the Stage
- Hook: Begin with a compelling question or statistic related to red blood cell health. This immediately grabs the reader’s attention. For example: "Did you know that your body creates and destroys millions of red blood cells every second? While natural, excessive destruction can lead to serious health problems."
- Define RBCs and Their Importance: Briefly explain what red blood cells (RBCs) are and their crucial role in oxygen transport. Keep it concise and accessible.
- Introduce the Concept of Hemolysis: Define hemolysis as the destruction of red blood cells. Briefly mention that this article will delve into the various reasons behind it.
- Keyword Integration: Naturally incorporate "RBC destruction causes" within the introduction without sounding forced.
- Outline the Scope: Briefly mention the types of causes the article will cover (e.g., inherited conditions, autoimmune disorders, etc.)
Causes Related to Inherited Conditions
- Introduction: Explain that some RBC destruction causes are inherited genetic disorders, affecting the structure or function of red blood cells.
- Hereditary Spherocytosis:
- Explanation: Describe this condition where RBCs are abnormally shaped (spherical) and easily destroyed.
- Genetic Basis: Briefly explain the genes involved and how mutations lead to spherocytosis.
- Symptoms: List common symptoms like anemia, jaundice, and enlarged spleen.
- Hereditary Elliptocytosis:
- Explanation: Describe this condition where RBCs are abnormally shaped (elliptical) and prone to destruction.
- Genetic Basis: Briefly explain the genes involved and how mutations lead to elliptocytosis.
- Symptoms: List common symptoms. Symptoms can range from being asymptomatic to having severe anemia.
- Sickle Cell Anemia:
- Explanation: Describe this condition where RBCs are crescent-shaped ("sickle-shaped") and fragile, leading to blockage and destruction.
- Genetic Basis: Explain the specific mutation in the hemoglobin gene (HBB) responsible.
- Symptoms: List common symptoms like pain crises, fatigue, and organ damage.
- Thalassemia:
- Explanation: Describe this group of disorders where the body produces abnormal hemoglobin, leading to RBC destruction.
- Types: Briefly describe alpha and beta thalassemia.
- Severity: Explain the range of severity, from mild to severe anemia.
- G6PD Deficiency:
- Explanation: Describe this enzyme deficiency that makes RBCs more vulnerable to oxidative stress and destruction.
- Triggering Factors: List common triggers like certain medications and infections.
- Symptoms: List common symptoms, often triggered by exposure to certain substances.
- Hereditary Spherocytosis:
Causes Related to Autoimmune Disorders
- Introduction: Explain that autoimmune disorders can cause the body to mistakenly attack and destroy its own red blood cells.
- Autoimmune Hemolytic Anemia (AIHA):
- Explanation: Describe AIHA as a condition where antibodies attack RBCs.
- Types: Differentiate between warm AIHA and cold AIHA, based on the temperature at which the antibodies are most active.
- Triggers: Mention possible triggers such as underlying infections or other autoimmune diseases.
- Symptoms: Explain common symptoms like fatigue, pale skin, and dark urine.
- Drug-Induced Hemolytic Anemia:
- Explanation: Explain that certain medications can trigger RBC destruction, sometimes through an autoimmune mechanism.
- Examples: Provide a few examples of drugs known to cause this.
- Mechanism: Briefly explain how the drugs may interact with RBCs or the immune system.
- Autoimmune Hemolytic Anemia (AIHA):
Causes Related to Infections
- Introduction: Explain that some infections can directly or indirectly damage RBCs, leading to their destruction.
- Malaria:
- Explanation: Describe how the malaria parasite infects and destroys RBCs.
- Geographic Distribution: Briefly mention the regions where malaria is prevalent.
- Symptoms: List common symptoms of malaria.
- Babesiosis:
- Explanation: Describe how this parasitic infection, transmitted by ticks, invades and damages RBCs.
- Symptoms: List common symptoms.
- Clostridium perfringens:
- Explanation: Explain that this bacteria, particularly during sepsis, can release toxins that destroy RBCs.
- Malaria:
Causes Related to Mechanical Destruction
- Introduction: Explain that physical forces can also cause RBC destruction.
- Microangiopathic Hemolytic Anemia (MAHA):
- Explanation: Describe how small blood clots (microthrombi) in the blood vessels can damage RBCs as they pass through.
- Associated Conditions: List conditions associated with MAHA, such as Thrombotic Thrombocytopenic Purpura (TTP), Hemolytic Uremic Syndrome (HUS), and Disseminated Intravascular Coagulation (DIC).
- Heart Valve Prosthesis:
- Explanation: Explain that artificial heart valves can sometimes damage RBCs due to shear stress.
- March Hemoglobinuria:
- Explanation: Describe how strenuous exercise, especially impact exercise (e.g., running), can damage RBCs in the feet, leading to hemoglobin in the urine.
- Microangiopathic Hemolytic Anemia (MAHA):
Causes Related to Chemical and Physical Agents
- Introduction: Explain that exposure to certain chemicals or physical agents can lead to RBC destruction.
- Exposure to Toxic Chemicals:
- Examples: List some examples of chemicals that can damage RBCs (e.g., lead, arsenic).
- Mechanism: Briefly explain how these chemicals affect RBCs.
- Severe Burns:
- Explanation: Explain that severe burns can directly damage RBCs.
- Hypophosphatemia:
- Explanation: Describe how a low level of phosphate in the blood can lead to RBC fragility and destruction.
- Exposure to Toxic Chemicals:
Diagnosis and Testing
- Introduction: Briefly explain how RBC destruction is diagnosed.
- Blood Smear: Describe how a blood smear can reveal abnormal RBC shapes or fragments (schistocytes).
- Complete Blood Count (CBC): Explain the role of CBC in detecting anemia (low RBC count).
- Reticulocyte Count: Explain how this test measures the bone marrow’s production of new RBCs in response to destruction.
- Lactate Dehydrogenase (LDH): Explain how elevated LDH levels can indicate tissue damage, including RBC destruction.
- Haptoglobin: Explain how low haptoglobin levels can indicate RBC destruction, as haptoglobin binds to free hemoglobin released during hemolysis.
- Bilirubin: Explain how elevated bilirubin levels can indicate RBC destruction.
- Direct Antiglobulin Test (DAT) or Coombs Test: Explain how this test is used to detect antibodies attached to RBCs in suspected AIHA.
Treatment Options
- Introduction: Briefly discuss the general approaches to treating RBC destruction, emphasizing that treatment varies widely depending on the underlying cause.
- Addressing the Underlying Cause: Emphasize that the primary focus is treating the root cause, such as managing an autoimmune disorder, treating an infection, or avoiding exposure to toxic substances.
- Blood Transfusions: Explain that blood transfusions may be necessary to treat severe anemia.
- Medications: Mention medications that may be used to suppress the immune system in AIHA or manage specific genetic disorders.
- Splenectomy: Explain that removing the spleen may be considered in some cases of AIHA or hereditary spherocytosis, as the spleen is a major site of RBC destruction.
- Supportive Care: Mention the importance of supportive care, such as maintaining adequate hydration and nutrition.
FAQs: Understanding RBC Destruction Causes
Here are some frequently asked questions to help you better understand the causes of red blood cell (RBC) destruction.
What does it mean when my doctor says I have increased RBC destruction?
It means your body is destroying red blood cells faster than it can produce them. This can lead to anemia, as your body doesn’t have enough healthy red blood cells to carry oxygen. Understanding rbc destruction causes is crucial for proper diagnosis and treatment.
What are some common rbc destruction causes?
Common causes include autoimmune disorders where your body attacks its own red blood cells, infections like malaria, genetic conditions such as sickle cell anemia and thalassemia, and exposure to certain drugs or toxins. Mechanical causes, like damaged heart valves, can also lead to rbc destruction.
How is increased RBC destruction diagnosed?
Diagnosis usually involves blood tests, including a complete blood count (CBC), peripheral blood smear, and Coombs test. These tests help determine the number of red blood cells, their shape, and whether antibodies are attacking them. Further investigations may be necessary to pinpoint the specific rbc destruction causes.
What are the treatment options for RBC destruction?
Treatment varies depending on the underlying cause. It may involve medications to suppress the immune system in autoimmune cases, antibiotics for infections, blood transfusions to increase red blood cell count, or in some cases, a splenectomy (removal of the spleen). Addressing the root rbc destruction causes is key to managing the condition.
So, that’s the lowdown on rbc destruction causes! Hope you found it helpful and now have a better grasp of what’s going on. Keep an eye on those red blood cells!