The pelvic bone, a crucial structure in the human body, features the pubic ramus, a bony extension contributing significantly to pelvic stability. The American Medical Association (AMA) recognizes the importance of understanding pubic ramus anatomy for accurate diagnosis and treatment of related conditions. Imaging techniques, such as X-rays and MRI, offer detailed visualization of the pubic ramus anatomy, aiding healthcare professionals in assessing fractures or abnormalities. Knowledge of pubic ramus anatomy is also essential for professionals in the field of physical therapy, enabling them to develop targeted rehabilitation plans for patients with injuries affecting the pelvic region.
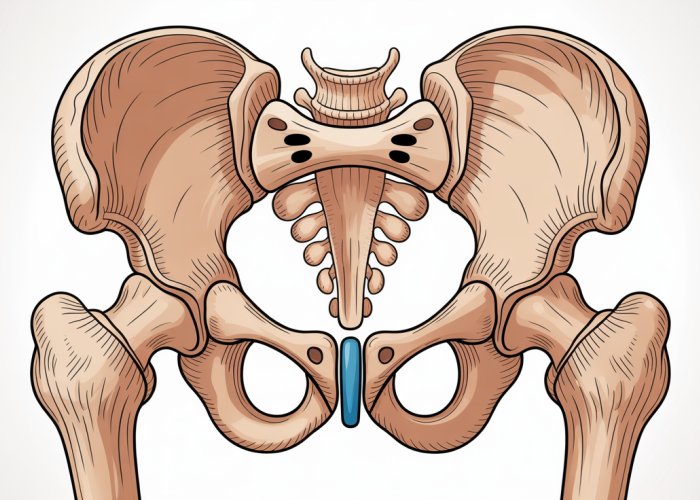
The pelvic girdle, a complex structure at the base of the spine, plays a pivotal role in human biomechanics and overall health.
Composed of paired hip bones (ilium, ischium, and pubis), the sacrum, and the coccyx, it serves as the foundation for the trunk, connecting the axial skeleton to the lower limbs.
The pelvic girdle supports the weight of the upper body, facilitates locomotion, and protects vital pelvic organs.
Within this intricate framework lies the pubic ramus, a critical component of the pubic bone.
The Pubic Ramus: A Key Component
The pubic ramus, a bony extension of the pubis, is divided into the superior and inferior rami.
These rami converge anteriorly at the pubic symphysis, a cartilaginous joint that provides stability and limited movement.
The pubic ramus contributes significantly to the structural integrity of the pelvis.
It serves as an attachment site for numerous muscles and ligaments essential for movement, posture, and pelvic stability.
Why Understanding the Pubic Ramus Matters
A thorough understanding of the pubic ramus anatomy is paramount for healthcare professionals across various disciplines.
From orthopedic surgeons and sports medicine physicians to radiologists and physical therapists, knowledge of its structure and function is crucial for accurate diagnosis, effective treatment planning, and successful rehabilitation of various conditions.
Clinical Significance
Injuries and pathologies affecting the pubic ramus can have a significant impact on a patient’s quality of life.
Fractures, often resulting from trauma or stress, can cause severe pain and limited mobility.
Nerve entrapment syndromes, such as obturator nerve entrapment, can lead to chronic groin pain and functional impairment.
Furthermore, pubic ramus abnormalities can contribute to pelvic instability and biomechanical dysfunction.
The Importance of Accurate Diagnosis
Accurate diagnosis is essential for effective management of pubic ramus-related conditions.
A comprehensive understanding of the anatomy, coupled with advanced diagnostic imaging techniques, enables healthcare professionals to identify the underlying cause of the patient’s symptoms.
This allows for the development of targeted treatment strategies.
These strategies aim to alleviate pain, restore function, and prevent long-term complications.
Implications for Treatment and Rehabilitation
Effective treatment and rehabilitation strategies for pubic ramus injuries require a detailed understanding of its anatomy and biomechanical role.
Surgical interventions, such as fracture fixation, may be necessary in severe cases.
Conservative management, including pain management and physical therapy, plays a crucial role in restoring strength, flexibility, and stability.
By understanding the intricate anatomy of the pubic ramus, healthcare professionals can optimize treatment outcomes and improve the overall well-being of their patients.
Injuries and pathologies affecting the pubic ramus can have a significant impact on a patient’s quality of life. Fractures, often resulting from trauma or stress, can cause severe pain and limited mobility. Nerve entrapment syndromes, such as obturator nerve entrapment, can lead to chronic pelvic pain and functional limitations. To fully grasp the impact of these conditions, it’s essential to delve into the intricate anatomical details of the pubic ramus and its surrounding structures.
Anatomy of the Pubic Ramus: A Detailed Look
The pubic ramus, an integral component of the pelvic girdle, plays a vital role in structural support, muscle attachments, and overall pelvic stability. A thorough understanding of its anatomy is crucial for healthcare professionals involved in the diagnosis and treatment of various pelvic conditions. Let’s examine the pubic ramus in detail.
The Pubis Bone: Foundation of the Ramus
The pubis bone forms the anterior and inferior portion of the hip bone (also known as the innominate bone or os coxae). It articulates with the ilium and ischium, contributing to the acetabulum (the hip socket). The pubis consists of a body, a superior ramus, and an inferior ramus. It’s the foundation upon which the pubic ramus is built.
The body of the pubis is the flattened, medial portion. This section articulates with the opposite pubis bone at the pubic symphysis.
Superior Pubic Ramus: Structure and Location
The superior pubic ramus extends laterally from the body of the pubis. It connects the pubis to the acetabulum, the socket that houses the head of the femur. This bony extension is located superiorly to the inferior pubic ramus.
The superior ramus forms the upper border of the obturator foramen, a large opening in the hip bone. It provides attachment sites for several important muscles, including the pectineus and adductor longus.
Inferior Pubic Ramus: Structure and Location
The inferior pubic ramus extends inferiorly and laterally from the body of the pubis. It joins with the ischial ramus to form the ischiopubic ramus. This ramus contributes to the lower border of the obturator foramen.
The inferior ramus provides attachment for muscles. This includes the adductor magnus and the gracilis, which are crucial for adduction and stabilization of the leg.
Pubic Symphysis: Connecting the Bones
The pubic symphysis is a cartilaginous joint. It is located at the anterior midline of the pelvis. It connects the left and right pubic bones. This joint is composed of fibrocartilage. It allows for slight movement, providing stability to the pelvic girdle.
During pregnancy, hormones like relaxin cause the ligaments surrounding the pubic symphysis to relax. This increasing the joint’s flexibility to facilitate childbirth.
Relationship to the Obturator Foramen
The obturator foramen is a large opening located in the hip bone. It is formed by the pubis and ischium. The pubic ramus contributes significantly to the boundaries of this foramen. The superior pubic ramus forms the upper border. The inferior pubic ramus forms the lower border.
The obturator nerve and vessels pass through the obturator foramen. The foramen supplies the adductor muscles of the thigh.
Relationship to the Acetabulum
The acetabulum is the cup-shaped socket on the lateral aspect of the hip bone. It articulates with the head of the femur to form the hip joint.
The superior pubic ramus contributes to the anterior and inferior portion of the acetabulum. This close proximity influences the biomechanics of the hip joint. The superior ramus transfers weight and forces during movement.
Function and Biomechanical Importance of the Pubic Ramus
Having explored the intricate anatomical landscape of the pubic ramus, we now turn our attention to its crucial role in the body’s overall function and biomechanics. The pubic ramus isn’t merely a structural component; it actively participates in providing support, facilitating movement, and safeguarding vital organs. Let’s delve into its multifaceted functions.
Structural Support within the Pelvic Bone
The pubic ramus is a cornerstone of pelvic girdle integrity.
It acts as a vital bridge, connecting the anterior and posterior aspects of the pelvis.
This connection is essential for maintaining the ring-like structure of the pelvis, which is crucial for stability.
The fusion of the superior and inferior rami provides a robust framework that withstands significant forces during movement and weight-bearing.
Any compromise to the integrity of the pubic ramus, such as a fracture, can significantly destabilize the entire pelvic girdle.
Muscle Attachments and Their Role in Movement and Stability
The pubic ramus serves as a crucial attachment point for numerous muscles.
These muscles are essential for movement of the hip, thigh, and trunk, as well as for maintaining pelvic stability.
Key muscles attaching to the pubic ramus include:
-
Adductor Muscles: These muscles (adductor longus, adductor brevis, gracilis) are responsible for drawing the thigh towards the midline of the body, playing a vital role in activities like walking, running, and maintaining balance.
-
Abdominal Muscles: Certain abdominal muscles, such as the rectus abdominis and the external oblique, have attachments near the pubic ramus, contributing to core stability and trunk flexion.
-
Pelvic Floor Muscles: Some pelvic floor muscles attach to the inferior pubic ramus. These muscles are vital for supporting pelvic organs, maintaining continence, and contributing to sexual function.
The precise placement and robust nature of these muscle attachments underscore the importance of the pubic ramus in facilitating coordinated and efficient movement.
Weight-Bearing and Locomotion
The pelvic girdle, including the pubic ramus, plays a significant role in weight-bearing.
It transfers weight from the upper body to the lower limbs during standing, walking, and running.
The pubic rami, in conjunction with the other pelvic bones, distribute these forces evenly.
This ensures that no single point bears excessive stress.
During locomotion, the pubic ramus facilitates efficient transfer of forces between the legs and the trunk.
A healthy pubic ramus is essential for maintaining a balanced and stable gait.
Protection of Pelvic Organs
Beyond structural support and movement, the pubic ramus contributes to the protection of delicate pelvic organs.
The bony structure of the pubic ramus, along with the other pelvic bones, forms a protective shield.
This shield safeguards organs such as the bladder, uterus (in females), ovaries (in females), and rectum.
By providing a physical barrier, the pubic ramus helps to minimize the risk of injury to these vital organs from external forces.
Functioning as an anchor for vital muscles and a critical component of the pelvic ring, the pubic ramus plays an integral role in locomotion, stability, and organ protection. However, this essential structure is not immune to injury and dysfunction.
Common Injuries and Conditions Affecting the Pubic Ramus
Like any bony structure, the pubic ramus is susceptible to a range of injuries and conditions that can significantly impact an individual’s quality of life. Among the most prevalent are fractures and obturator nerve entrapment, each with its own unique set of causes, symptoms, and management strategies. Understanding these conditions is crucial for accurate diagnosis and effective treatment.
Pubic Ramus Fractures
Fractures of the pubic ramus represent a significant source of pain and disability, particularly in elderly populations and athletes. These fractures can occur as a result of high-impact trauma or repetitive stress.
Causes of Pubic Ramus Fractures
Pubic ramus fractures can broadly be categorized into traumatic fractures and stress fractures. Traumatic fractures typically result from a direct blow to the pelvis, such as in a motor vehicle accident or a fall from height. The high energy involved in these injuries can lead to significant displacement of the fracture fragments and potential damage to surrounding soft tissues.
Stress fractures, on the other hand, are more insidious in onset.
They occur due to repetitive microtrauma, often seen in athletes involved in endurance sports like long-distance running.
Osteoporosis, a condition characterized by decreased bone density, significantly increases the risk of stress fractures of the pubic ramus, especially in older adults. Even minor falls or everyday activities can lead to fractures in individuals with weakened bones.
Symptoms of Pubic Ramus Fractures
The hallmark symptom of a pubic ramus fracture is pain in the groin, hip, or lower back. This pain is often exacerbated by weight-bearing activities, such as walking or standing.
Patients may also experience limited mobility due to the pain and instability caused by the fracture.
Other common symptoms include:
- Tenderness to palpation over the pubic ramus.
- Pain with hip movement.
- Difficulty walking or bearing weight on the affected side.
- In some cases, bruising or swelling in the groin area.
Diagnosis of Pubic Ramus Fractures
A thorough clinical examination, combined with appropriate imaging studies, is essential for accurately diagnosing pubic ramus fractures.
X-rays are typically the first-line imaging modality.
They can often visualize displaced fractures.
However, stress fractures or non-displaced fractures may be difficult to detect on plain radiographs.
CT scans provide more detailed images of the bony structures and are particularly useful for identifying subtle fractures or assessing the extent of fracture displacement.
MRI is the most sensitive imaging modality for detecting stress fractures.
It can also help evaluate associated soft tissue injuries, such as muscle strains or ligament sprains.
Treatment Options for Pubic Ramus Fractures
The treatment of pubic ramus fractures depends on the severity and stability of the fracture, as well as the patient’s overall health and activity level.
Most stable, non-displaced fractures can be managed conservatively with:
- Pain Management (Analgesics).
- Rest.
- Protected weight-bearing.
- Physical Therapy.
Pain medications, such as acetaminophen or NSAIDs, can help alleviate pain and inflammation. Physical therapy plays a crucial role in restoring strength, flexibility, and function.
In cases of displaced or unstable fractures, surgical intervention may be necessary to restore the integrity of the pelvic ring. Surgical options include:
- Open Reduction and Internal Fixation (ORIF).
- Percutaneous screw fixation.
These procedures aim to realign the fracture fragments and stabilize them with plates, screws, or rods.
Obturator Nerve Entrapment
The obturator nerve, which originates in the lumbar spine and passes through the pelvis, can sometimes become compressed or entrapped near the pubic ramus.
This can result in a range of neurological symptoms.
Causes of Obturator Nerve Entrapment
Several factors can contribute to obturator nerve entrapment, including:
- Trauma: Pelvic fractures or dislocations can directly injure or compress the nerve.
- Scar tissue: Following surgery or injury, scar tissue formation can encase the nerve, leading to entrapment.
- Tumors or masses: Rarely, tumors or other space-occupying lesions in the pelvis can compress the obturator nerve.
- Pregnancy: The expanding uterus during pregnancy can put pressure on the nerve.
- Repetitive activities: Activities that involve repetitive hip adduction or external rotation can irritate the nerve.
Symptoms of Obturator Nerve Entrapment
The primary symptom of obturator nerve entrapment is pain in the groin, medial thigh, or knee.
The pain is often described as:
- Aching.
- Burning.
- Shooting.
Other common symptoms include:
- Weakness in the hip adductor muscles.
- Difficulty with activities that require hip adduction, such as squeezing the knees together.
- Numbness or tingling in the medial thigh.
- In severe cases, difficulty walking or maintaining balance.
Treatment of Obturator Nerve Entrapment
The treatment for obturator nerve entrapment aims to relieve pressure on the nerve and restore its function.
Conservative management options include:
- Physical therapy: Stretching and strengthening exercises can help improve hip mobility and reduce nerve compression.
- Pain medications: Analgesics, such as NSAIDs or nerve pain medications like gabapentin, can help alleviate pain.
- Injections: Corticosteroid injections near the nerve can reduce inflammation and provide temporary pain relief.
In cases where conservative treatment fails to provide adequate relief, surgical decompression of the obturator nerve may be considered. This involves releasing any constricting tissues around the nerve.
Diagnostic Imaging of the Pubic Ramus
When pain arises in the pelvic region, pinpointing the source can be a complex undertaking. Fortunately, advancements in medical imaging provide clinicians with powerful tools to visualize the pubic ramus and assess its condition with remarkable precision. From identifying fractures to evaluating soft tissue damage, these techniques are indispensable for accurate diagnosis and effective treatment planning.
X-ray Techniques for Pubic Ramus Visualization
Plain radiography, commonly known as X-ray, remains the initial and often most accessible imaging modality for evaluating suspected pubic ramus injuries.
Standard anteroposterior (AP) pelvic views offer a broad overview of the bony structures, allowing for the detection of obvious fractures or dislocations.
However, subtle fractures, particularly stress fractures, may be difficult to visualize on standard X-rays, especially in the early stages.
Additional specialized views, such as the Judet views (oblique views of the pelvis), may be employed to better visualize the acetabulum and surrounding structures, potentially revealing fractures that are not apparent on the AP view.
While X-rays are excellent for assessing bony alignment and detecting gross fractures, they offer limited information about soft tissues. This limitation underscores the need for complementary imaging techniques in certain cases.
CT Scans: Detailed Assessment of Bone Structure
Computed Tomography (CT) scans provide a more detailed assessment of the bony architecture of the pubic ramus compared to plain radiographs.
CT imaging utilizes X-rays in conjunction with sophisticated computer processing to generate cross-sectional images of the body. These images can then be reconstructed in multiple planes, providing a three-dimensional representation of the bone.
This enhanced visualization is particularly useful for identifying complex fractures, fracture displacement, and associated injuries to the pelvic ring.
Advantages of CT Scanning
CT scans are highly sensitive for detecting fractures, even those that are subtle or non-displaced. The cross-sectional images allow for a precise assessment of fracture morphology, which is crucial for surgical planning.
In cases of high-energy trauma, CT scans can also help to identify associated injuries to adjacent structures, such as the bladder, bowel, or blood vessels.
Limitations of CT Scanning
The primary drawback of CT scanning is the exposure to ionizing radiation. While the radiation dose is generally considered to be low, it is important to weigh the benefits of the scan against the potential risks, especially in younger patients. CT scans also offer limited information about soft tissues, making them less useful for evaluating nerve entrapment or muscle injuries.
MRI: Evaluating Soft Tissues and Stress Fractures
Magnetic Resonance Imaging (MRI) provides superior visualization of soft tissues compared to X-rays and CT scans. MRI uses strong magnetic fields and radio waves to create detailed images of the body’s internal structures.
Unlike X-rays and CT scans, MRI does not involve ionizing radiation, making it a safer alternative for certain patient populations, such as pregnant women and children (although precautions are still taken).
Role of MRI in Pubic Ramus Injuries
MRI is particularly useful for evaluating suspected stress fractures of the pubic ramus, which may be difficult to detect on plain radiographs.
Stress fractures often present with bone marrow edema, a subtle finding that is easily visualized on MRI.
MRI is also valuable for assessing associated soft tissue injuries, such as muscle strains, ligament tears, and obturator nerve entrapment. The ability to visualize these structures directly allows for a more accurate diagnosis and targeted treatment.
Limitations of MRI
MRI scans are more expensive and time-consuming than X-rays or CT scans. They may also be contraindicated in patients with certain metallic implants or devices. Claustrophobia can also be a limiting factor, although open MRI scanners are available in some facilities.
CT scans offer an incredibly detailed look at the bone structure, revealing even hairline fractures with precision. MRI goes a step further, offering insights into soft tissue damage and subtle stress fractures that might be missed by other methods. With a clear picture of what’s happening inside, the next step is determining the best path to recovery.
Treatment and Management Strategies for Pubic Ramus Injuries
Once a pubic ramus injury has been diagnosed, a comprehensive treatment plan is essential to facilitate healing, restore function, and alleviate pain. Management strategies range from conservative, non-surgical approaches to more invasive surgical interventions, depending on the severity and nature of the injury. The ultimate goal is to return the individual to their pre-injury activity level with minimal long-term complications.
Non-Surgical Pain Management
For many pubic ramus injuries, particularly stress fractures or minor fractures without significant displacement, non-surgical pain management is the cornerstone of treatment. This approach focuses on reducing pain and inflammation, allowing the body’s natural healing processes to take over.
Rest and Activity Modification
Rest is paramount in the initial stages of recovery. This often involves limiting weight-bearing activities and avoiding movements that exacerbate pain. Crutches or other assistive devices may be necessary to facilitate mobility while minimizing stress on the pubic ramus.
Activity modification is also crucial. This means temporarily avoiding high-impact activities, such as running or jumping, and gradually reintroducing them as pain subsides and healing progresses.
Pharmacological Interventions
Over-the-counter pain relievers, such as acetaminophen (Tylenol) or nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen (Advil, Motrin) or naproxen (Aleve), can be effective in managing mild to moderate pain.
NSAIDs not only alleviate pain but also reduce inflammation, which is a common component of pubic ramus injuries.
In cases of more severe pain, a physician may prescribe stronger pain medications, such as opioid analgesics. However, these medications should be used with caution due to their potential for side effects and dependence.
Other Non-Surgical Modalities
Ice and heat therapy can also play a role in pain management. Ice packs applied to the affected area can help reduce inflammation and numb the pain, while heat can promote blood flow and muscle relaxation.
Supportive devices, such as pelvic binders, can provide stability and reduce pain by limiting movement of the pubic ramus.
The Role of Physical Therapy in Rehabilitation
Physical therapy is an integral part of the rehabilitation process for pubic ramus injuries. A skilled physical therapist can design a customized exercise program to restore strength, flexibility, and range of motion.
Early-Stage Rehabilitation
In the initial stages, physical therapy focuses on gentle exercises to maintain mobility and prevent stiffness. These may include range-of-motion exercises for the hip and knee, as well as isometric exercises to strengthen the surrounding muscles without placing excessive stress on the pubic ramus.
Progressive Strengthening and Functional Exercises
As healing progresses, the physical therapy program gradually intensifies. Strengthening exercises are introduced to target the muscles of the hip, pelvis, and core, which play a crucial role in supporting the pubic ramus and maintaining stability.
Functional exercises, such as walking, stair climbing, and squatting, are incorporated to simulate real-life activities and prepare the individual for a return to their pre-injury level of function.
Importance of Core Stability
Core stability is particularly important in the rehabilitation of pubic ramus injuries. A strong core provides a stable base of support for the pelvis and spine, reducing stress on the pubic ramus and improving overall biomechanics.
Physical therapists often incorporate exercises that target the deep core muscles, such as the transverse abdominis and multifidus, to enhance core stability and prevent future injuries.
Surgical Interventions for Severe Fractures
While most pubic ramus injuries can be effectively managed with non-surgical treatments, surgical intervention may be necessary in cases of severe fractures, particularly those involving significant displacement or instability.
Indications for Surgery
Surgery is typically considered when:
- The fracture is significantly displaced, meaning the bone fragments are not properly aligned.
- The fracture is unstable, meaning it is likely to shift or move during healing.
- There are associated injuries, such as damage to blood vessels or nerves.
- Non-surgical treatments have failed to provide adequate pain relief or stability.
Surgical Procedures
The specific surgical procedure will depend on the type and severity of the fracture. Common surgical techniques include:
- Open Reduction and Internal Fixation (ORIF): This involves making an incision to expose the fracture site, realigning the bone fragments, and securing them in place with plates, screws, or rods.
- Percutaneous Fixation: This minimally invasive technique involves inserting screws or pins through small incisions to stabilize the fracture.
- External Fixation: This involves placing pins or screws through the skin and into the bone, which are then connected to an external frame. This provides stability to the fracture while it heals.
Post-operative Care
Following surgery, a period of rehabilitation is essential to regain strength, flexibility, and function. This typically involves a structured physical therapy program, as well as pain management strategies.
The recovery time following surgery for a pubic ramus fracture can vary depending on the individual and the complexity of the fracture, but it often takes several months to achieve full recovery.
Frequently Asked Questions About Pubic Ramus Anatomy
Hopefully, this article provided a clear understanding of the pubic ramus. Here are some frequently asked questions to further clarify some common points of confusion.
What exactly is the pubic ramus?
The pubic ramus is a bony extension that forms part of the pelvis. Specifically, it’s a section of the pubic bone which itself is a part of the os coxae. Understanding pubic ramus anatomy is crucial for orthopedic surgeons and anyone studying human anatomy.
What is the difference between the superior and inferior pubic ramus?
The superior pubic ramus extends from the pubic body towards the acetabulum (hip socket). The inferior pubic ramus extends downward and backward to connect with the ischium. Both are integral components of pubic ramus anatomy.
What are the main functions of the pubic ramus?
The pubic ramus provides attachment points for muscles and ligaments crucial for hip and thigh movement. It also contributes to the overall structural integrity of the pelvis, playing a vital role in weight-bearing. Proper pubic ramus anatomy is essential for biomechanical function.
What types of injuries can occur to the pubic ramus?
Fractures are the most common injuries affecting the pubic ramus. These can occur due to high-impact trauma, falls, or stress fractures, particularly in athletes. Imaging techniques are used to assess the specific nature and extent of pubic ramus anatomy injuries.
So, there you have it – a quick rundown of pubic ramus anatomy! Hopefully, this helps you understand a little more about how your body works. Keep exploring, keep asking questions, and remember to consult with a healthcare professional for any specific concerns you have about your pubic ramus anatomy. Take care!