Understanding the intricate function of the kidney requires a thorough grasp of its microvasculature. Peritubular capillaries definition hinges on their crucial role in renal physiology, specifically their interaction with the renal tubules, where reabsorption and secretion processes occur. Their proximity to the proximal and distal convoluted tubules, along with the Loop of Henle, enables efficient exchange of substances vital for maintaining fluid and electrolyte balance. Furthermore, glomerular filtration rate, a key indicator of kidney function, is indirectly influenced by the pressure and flow dynamics within the peritubular capillaries, highlighting the interconnectedness of the kidney’s filtration and reabsorption systems. Nephrology specialists extensively study these capillaries to diagnose and manage various renal diseases.
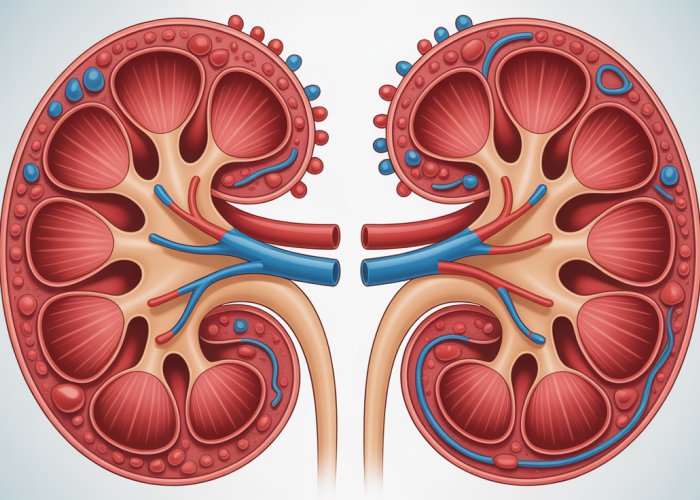
The kidney, a remarkable organ, stands as a central pillar in the body’s intricate system of maintaining homeostasis.
Its bean-shaped structure belies its complex functionality, tirelessly working to filter blood, regulate fluid balance, and excrete waste products.
Central to this process is the nephron, the kidney’s functional unit.
This microscopic structure, numbering in the millions within each kidney, orchestrates the critical tasks of filtration, reabsorption, and secretion.
Within the nephron’s intricate architecture lies a network of tiny blood vessels known as the peritubular capillaries.
The Renal Microvasculature: A Closer Look
These capillaries, often overlooked, are essential components of the renal microvasculature. They intimately interact with the renal tubules.
They play a pivotal role in the exchange of vital substances.
Understanding their function is key to comprehending overall kidney health.
Purpose of this Article
This article aims to provide a comprehensive exploration of peritubular capillaries.
We seek to define their structure, explain their function, and highlight their clinical significance.
By delving into the intricacies of these tiny vessels, we hope to shed light on their crucial contribution to renal physiology and overall health.
The intricate dance between the nephron and its associated vasculature is crucial for proper kidney function. While the nephron handles filtration, reabsorption, and secretion, the surrounding blood vessels, particularly the peritubular capillaries, are the unsung heroes facilitating these processes. Understanding the architecture and arrangement of these tiny vessels is key to appreciating their role in maintaining overall health.
Defining Peritubular Capillaries: Structure and Location
Peritubular capillaries are a complex network of tiny blood vessels that intimately surround the renal tubules within the kidney. These capillaries are not randomly dispersed but rather strategically positioned to maximize their interaction with the nephron’s various segments.
Origin and Anatomical Position
Peritubular capillaries originate from the efferent arteriole, the vessel carrying blood away from the glomerulus after filtration has occurred. Unlike the afferent arteriole, which supplies blood to the glomerulus, the efferent arteriole doesn’t directly lead back to a larger artery.
Instead, it branches out into this extensive network of capillaries.
These capillaries then weave their way around the proximal convoluted tubule (PCT), the distal convoluted tubule (DCT), and portions of the loop of Henle, facilitating the exchange of substances between the tubular fluid and the bloodstream.
This close proximity is essential for the kidney’s ability to selectively reabsorb vital nutrients and water while simultaneously secreting waste products and toxins.
Peritubular Capillaries vs. Vasa Recta
Within the renal vasculature, it is crucial to distinguish peritubular capillaries from the vasa recta, another specialized capillary network. While both types of vessels are found in the kidney, they serve distinct functions and have different anatomical arrangements.
The key difference lies in their location and the nephron segments they associate with. Vasa recta are long, straight capillaries that primarily follow the loop of Henle deep into the renal medulla.
This arrangement is particularly important for the concentration of urine. By contrast, peritubular capillaries are predominantly found in the renal cortex, surrounding the PCT and DCT.
They play a more direct role in the reabsorption and secretion processes occurring in these segments. While both capillary networks are vital for overall kidney function, they serve different aspects of renal physiology, highlighting the organ’s structural and functional complexity.
The distinctions between peritubular capillaries and vasa recta illuminate the kidney’s functional specialization. Now, let’s turn our attention to the pivotal roles these delicate vessels play in the core processes of renal function: reabsorption and secretion.
The Crucial Role in Renal Function: Reabsorption and Secretion
The peritubular capillaries and renal tubules operate in a tightly coupled manner, orchestrating the kidney’s remarkable ability to filter, refine, and regulate the composition of our internal environment. This intricate relationship is the foundation of reabsorption and secretion, two processes vital for maintaining homeostasis.
Reabsorption: Retrieving Essential Substances
Reabsorption is the process by which water and solutes are transported from the tubular fluid back into the bloodstream. The peritubular capillaries are indispensable to this process.
They act as the receiving vessels for the substances reclaimed from the filtrate. As the filtrate flows through the proximal convoluted tubule (PCT), loop of Henle, and distal convoluted tubule (DCT), water, electrolytes (such as sodium, potassium, and chloride), and essential nutrients (like glucose and amino acids) are selectively transported out of the tubular fluid.
The peritubular capillaries, with their close proximity to the tubules, readily absorb these reclaimed substances, returning them to the systemic circulation.
The Role of Renal Blood Flow in Reabsorption
Renal blood flow directly impacts the efficiency of reabsorption. Adequate blood flow ensures that the peritubular capillaries can effectively remove reabsorbed substances, maintaining a concentration gradient that favors further reabsorption from the tubular fluid.
Reduced renal blood flow can impair reabsorption, leading to the loss of essential nutrients and electrolytes in the urine. This is why conditions affecting renal blood flow often manifest with electrolyte imbalances and other metabolic disturbances.
Secretion: Eliminating Waste Products
Secretion is the opposite of reabsorption; it involves the transport of substances from the blood into the tubular fluid. The peritubular capillaries play a crucial role in this process as well.
They deliver waste products, toxins, and excess ions to the renal tubules for excretion. Substances such as creatinine, urea, certain drugs, and hydrogen ions are actively secreted from the peritubular capillaries into the tubular fluid.
This process allows the kidneys to eliminate harmful substances and fine-tune the balance of electrolytes and pH in the body.
The Role of Renal Blood Flow in Secretion
Just as with reabsorption, renal blood flow is critical for efficient secretion. Adequate blood flow ensures that the peritubular capillaries can effectively deliver waste products to the tubules for excretion.
Impaired renal blood flow can hinder secretion, leading to the accumulation of toxins and waste products in the blood.
Maintaining the Interstitial Fluid Environment
Beyond reabsorption and secretion, the peritubular capillaries contribute to maintaining the delicate balance of the interstitial fluid environment surrounding the renal tubules.
By regulating the movement of water and solutes, these capillaries help maintain the proper osmotic pressure and composition of the interstitial fluid, which is essential for optimal tubular function.
This is crucial for the efficient transport of substances across the tubular epithelium. The peritubular capillaries’ ability to maintain this balance is essential for the overall health and function of the kidneys.
The kidney’s ability to selectively reclaim valuable substances and excrete waste hinges on the continuous interplay between renal tubules and their adjacent capillary networks. This dynamic exchange, meticulously governed by the peritubular capillaries and vasa recta, is not merely about waste disposal; it’s intrinsically linked to the body’s broader homeostatic mechanisms.
Connection to Renal Physiology: Maintaining Balance
Beyond their direct roles in reabsorption and secretion, peritubular capillaries are deeply intertwined with the overall renal physiology, playing a vital role in maintaining systemic equilibrium. These tiny vessels are key players in regulating blood pressure, electrolyte and acid-base balance, and even the production of red blood cells through erythropoietin.
Blood Pressure Regulation
The peritubular capillaries play an indirect but crucial role in blood pressure regulation through the renin-angiotensin-aldosterone system (RAAS). Specialized cells in the kidney, specifically the juxtaglomerular cells, sense changes in renal blood flow and pressure.
When blood pressure drops, these cells release renin, initiating a cascade of hormonal events. This ultimately leads to the production of angiotensin II, a potent vasoconstrictor that increases blood pressure.
Angiotensin II also stimulates the release of aldosterone from the adrenal glands, which promotes sodium and water reabsorption in the distal tubules and collecting ducts, further increasing blood volume and pressure. The peritubular capillaries are essential for delivering angiotensin II and aldosterone to their target sites within the kidney and for reabsorbing the increased sodium and water, thereby completing the feedback loop.
Electrolyte Balance
The kidney’s ability to maintain electrolyte balance is critically dependent on the peritubular capillaries. As electrolytes like sodium, potassium, calcium, and phosphate are filtered and reabsorbed along the nephron, the peritubular capillaries ensure their efficient return to the systemic circulation, preventing excessive loss or accumulation.
The reabsorption of sodium, in particular, is closely linked to water reabsorption and blood pressure regulation. The peritubular capillaries maintain the osmotic gradient that drives water movement, facilitating the fine-tuning of sodium levels in the blood. Dysfunction of these capillaries can disrupt electrolyte balance, leading to conditions such as hyponatremia (low sodium) or hyperkalemia (high potassium), with potentially severe consequences for cellular function and cardiac rhythm.
Acid-Base Balance
Maintaining a stable blood pH is essential for enzyme function and overall cellular health. The kidneys play a critical role in acid-base balance by excreting excess acids or bases and by reabsorbing bicarbonate, a crucial buffer.
The peritubular capillaries are essential for transporting the secreted acids and bases into the tubular fluid for excretion and for returning the reabsorbed bicarbonate to the bloodstream. The enzyme carbonic anhydrase, present in both the tubular cells and the peritubular capillaries, plays a crucial role in this process, catalyzing the conversion of carbon dioxide and water into bicarbonate and hydrogen ions.
Disruptions in peritubular capillary function can impair the kidney’s ability to regulate acid-base balance, leading to metabolic acidosis or alkalosis.
Erythropoietin Production
The peritubular capillaries also play a vital role in regulating the production of red blood cells through the hormone erythropoietin (EPO). Specialized cells in the kidney, located near the peritubular capillaries, sense oxygen levels in the blood.
When oxygen levels are low (hypoxia), these cells release EPO, which stimulates red blood cell production in the bone marrow. The peritubular capillaries are essential for delivering EPO to the bone marrow and for transporting the newly produced red blood cells into the circulation.
Chronic kidney disease, which often involves damage to the peritubular capillaries, can impair EPO production, leading to anemia. This anemia contributes significantly to the morbidity and mortality associated with kidney disease.
Clinical Significance: Peritubular Capillaries and Renal Disease
The intricate dance between peritubular capillaries and renal tubules, as we’ve seen, is paramount for maintaining homeostasis. But what happens when this delicate system falters? The answer lies in a cascade of clinical consequences, highlighting the vulnerability of these tiny vessels and their profound impact on renal health.
Dysfunction within the peritubular capillaries can be a critical contributor to the pathogenesis and progression of various renal diseases. The health of these capillaries is inextricably linked to the overall function of the nephron, and any compromise can lead to significant renal impairment.
The Impact of Capillary Damage on Kidney Function
When the peritubular capillaries are damaged or dysfunctional, the kidney’s ability to effectively reabsorb essential substances and secrete waste products is severely compromised. This leads to a buildup of toxins in the bloodstream and an imbalance of vital electrolytes.
Ischemic injury, a reduction in blood supply, can directly damage the capillaries, leading to cell death and fibrosis. This, in turn, reduces the surface area available for reabsorption and secretion, further exacerbating renal dysfunction.
The consequences of this dysfunction are far-reaching, contributing to the development or worsening of chronic kidney disease (CKD), acute kidney injury (AKI), and other renal disorders.
Hypertension’s Toll on Peritubular Health
Hypertension, a prevalent systemic condition, exerts a significant influence on the health and function of peritubular capillaries. Chronic high blood pressure can lead to glomerular hypertension, which is then transmitted to the peritubular capillaries, causing structural damage.
This damage can manifest as capillary rarefaction, a decrease in the number of capillaries, as well as endothelial dysfunction, impairing their ability to regulate blood flow and permeability. The altered capillary structure and function then reduce the efficiency of reabsorption and secretion processes.
Furthermore, hypertension can accelerate the progression of kidney disease by promoting fibrosis and scarring within the renal tissue. This creates a vicious cycle, where kidney damage leads to further increases in blood pressure, perpetuating the injury.
Medications and Peritubular Capillary Integrity
Certain medications can also exert adverse effects on the peritubular capillaries, impacting their structure and function. Nonsteroidal anti-inflammatory drugs (NSAIDs), for instance, can constrict afferent arterioles, reducing blood flow to the glomerulus and subsequently affecting the peritubular capillaries.
Similarly, some immunosuppressants, such as cyclosporine and tacrolimus, can cause vasoconstriction and endothelial dysfunction, leading to impaired capillary function and an increased risk of kidney damage.
It is crucial to consider the potential nephrotoxic effects of medications, particularly in patients with pre-existing renal conditions or those at risk of developing kidney disease.
Tubule-Specific Conditions and Capillary Dependence
The function of each segment of the renal tubule – the Proximal Convoluted Tubule (PCT), Distal Convoluted Tubule (DCT), Loop of Henle, and Collecting Duct – is intricately linked to the health and proper functioning of the surrounding peritubular capillaries.
-
Proximal Convoluted Tubule (PCT): The PCT is responsible for the reabsorption of the majority of filtered glucose, amino acids, and bicarbonate. This energy-intensive process relies heavily on adequate oxygen and nutrient delivery via the peritubular capillaries. Damage to these capillaries can lead to impaired PCT function, resulting in glycosuria, aminoaciduria, and metabolic acidosis.
-
Loop of Henle: The Loop of Henle establishes the medullary concentration gradient, which is essential for water reabsorption. The vasa recta, specialized peritubular capillaries within the medulla, play a crucial role in maintaining this gradient. Dysfunction of the vasa recta can disrupt the concentration gradient, leading to impaired water reabsorption and polyuria.
-
Distal Convoluted Tubule (DCT): The DCT is involved in the fine-tuning of electrolyte balance, particularly sodium and potassium. Aldosterone, a hormone that promotes sodium reabsorption and potassium secretion, acts on the DCT. The peritubular capillaries are essential for delivering aldosterone to the DCT and for reabsorbing the sodium that is reabsorbed by this segment.
-
Collecting Duct: The collecting duct is the final site of water reabsorption in the nephron. Antidiuretic hormone (ADH), also known as vasopressin, acts on the collecting duct to increase water permeability. The peritubular capillaries surrounding the collecting duct are essential for reabsorbing the water that is reabsorbed under the influence of ADH. Damage can lead to nephrogenic diabetes insipidus, characterized by the inability to concentrate urine.
In essence, a healthy capillary network is essential for each segment’s specialized tasks. Any disruption in this network can have cascading effects, leading to specific clinical manifestations related to the affected tubule segment.
Hypertension’s relentless assault on the delicate renal vasculature serves as a stark reminder that even seemingly minor imbalances can trigger a cascade of detrimental effects. The peritubular capillaries, with their critical role in renal function, are particularly vulnerable to the damaging effects of elevated blood pressure. This can lead to structural damage and ultimately compromise the kidney’s ability to maintain homeostasis.
Factors Affecting Peritubular Capillary Function: A Delicate Balance
The function of peritubular capillaries is not a static process. It is a carefully orchestrated balance influenced by a multitude of factors. Understanding these factors is crucial to appreciating the vulnerability of these capillaries and their susceptibility to dysfunction. Renal blood flow, interstitial fluid pressure, and endothelial function each play a significant role in determining the efficiency of reabsorption and secretion. Disruptions in any of these areas can have far-reaching consequences for overall renal health.
The Impact of Renal Blood Flow
Renal blood flow is the lifeline of the kidney. It directly dictates the rate at which substances are delivered to and removed from the peritubular capillaries. Changes in renal blood flow can have a profound impact on the function of these capillaries.
Increased blood flow, for instance, enhances the delivery of solutes to the capillaries, potentially increasing both reabsorption and secretion rates. However, excessive blood flow can overwhelm the capillaries, reducing the efficiency of these processes.
Conversely, decreased blood flow, as seen in conditions like renal artery stenosis, can lead to ischemia and reduced delivery of essential nutrients and oxygen to the tubular cells. This compromises their ability to perform reabsorption and secretion effectively. Furthermore, reduced blood flow slows the removal of waste products. This can lead to their buildup in the interstitium, further impairing capillary function.
Ultimately, maintaining optimal renal blood flow is paramount for supporting the vital functions of the peritubular capillaries. Any significant deviation from this optimal range can disrupt the delicate balance of reabsorption and secretion.
Interstitial Fluid Pressure Dynamics
The pressure within the interstitial fluid, the fluid surrounding the renal tubules and peritubular capillaries, plays a critical role in regulating the movement of fluids and solutes across the capillary walls.
An increase in interstitial fluid pressure, for example, can impede the reabsorption of fluids back into the capillaries. This occurs because the elevated pressure opposes the osmotic forces driving reabsorption. Conditions like kidney inflammation (nephritis) can increase interstitial fluid pressure, leading to fluid retention and edema.
Conversely, a decrease in interstitial fluid pressure can enhance reabsorption. However, excessively low pressure can compromise the structural integrity of the interstitium and impair overall renal function.
Therefore, maintaining an appropriate interstitial fluid pressure is essential for optimizing the reabsorptive capacity of the peritubular capillaries and preventing fluid imbalances.
Endothelial Dysfunction and Capillary Permeability
The endothelium, the inner lining of the peritubular capillaries, acts as a selective barrier, controlling the passage of substances between the blood and the interstitial fluid. Endothelial dysfunction, characterized by damage or impaired function of these cells, can significantly alter capillary permeability.
This increased permeability allows proteins and other large molecules to leak out of the capillaries into the interstitium. This not only reduces the oncotic pressure within the capillaries, hindering reabsorption. It also contributes to inflammation and fibrosis in the interstitium, further impairing renal function.
Conditions like diabetes, hypertension, and chronic inflammation can all contribute to endothelial dysfunction in the peritubular capillaries. Addressing these underlying conditions is crucial for preserving endothelial integrity and maintaining optimal capillary function.
Peritubular Capillaries: Frequently Asked Questions
Want to understand the importance of peritubular capillaries better? Here are some common questions about this crucial part of the kidney’s filtration system.
What exactly are peritubular capillaries?
Peritubular capillaries are tiny blood vessels that surround the convoluted tubules and loop of Henle in the nephron of the kidney. These capillaries play a vital role in reabsorbing essential substances back into the bloodstream after initial filtration. Understanding the peritubular capillaries definition is key to grasping kidney function.
What is the main function of these capillaries?
The primary function is to reabsorb water, ions, glucose, amino acids, and other nutrients from the filtrate back into the blood. This process prevents these essential substances from being lost in urine. The peritubular capillaries definition highlights their importance in conserving resources.
How do peritubular capillaries differ from glomerular capillaries?
Glomerular capillaries are responsible for the initial filtration of blood, pushing fluid and small solutes into Bowman’s capsule. Peritubular capillaries, on the other hand, reabsorb substances from the filtrate back into the bloodstream. The peritubular capillaries definition focuses on their role in reabsorption, contrasting with the glomerular filtration role.
Why are peritubular capillaries so important for kidney health?
These capillaries ensure that valuable nutrients and water are not wasted, maintaining fluid and electrolyte balance in the body. Damage or dysfunction of these capillaries can significantly impair kidney function. Understanding the peritubular capillaries definition is critical for understanding kidney health.
So, now you’ve got the scoop on the peritubular capillaries definition and their importance in your kidneys! Hope this helped clear things up. Keep those kidneys happy!