Bone remodeling, a vital process managed by osteoclasts and osteoblasts within the bone matrix, is fundamentally linked to the structural organization of bone. This intricate architecture centers around the Haversian system, the primary component of compact bone. Understanding the definition of osteon is essential for grasping the mechanical strength and physiological functionality of skeletal tissue. This article provides an in-depth exploration into the anatomy, physiology, and clinical relevance of the osteon.
Bone, far from being the static, inert material we often perceive, is a dynamic and complex tissue, constantly adapting and remodeling itself throughout our lives. Understanding its intricate structure is not merely an academic exercise; it’s crucial for comprehending overall health, from preventing fractures to managing metabolic diseases.
At the heart of compact bone lies a remarkable structural unit: the osteon, also known as the Haversian System. This microscopic marvel is the fundamental building block that provides bone with its strength and resilience.
This article embarks on a journey into the microscopic world of bone, with the central aim of providing a comprehensive definition of the osteon and exploring its multifaceted components. By delving into its anatomy and function, we aim to illuminate the vital role it plays in skeletal health.
Bone: A Dynamic and Complex Tissue
Bone tissue is continuously undergoing a process of formation and resorption, responding to mechanical stress, hormonal signals, and nutritional factors. This dynamic nature allows bone to adapt to changing demands and repair damage.
The complexity of bone extends to its cellular composition, which includes osteoblasts (bone-forming cells), osteocytes (mature bone cells), and osteoclasts (bone-resorbing cells), all working in concert to maintain skeletal integrity.
The Importance of Understanding Bone Structure
A thorough understanding of bone structure is essential for several reasons:
- Diagnosing and treating bone diseases: Conditions like osteoporosis, osteomalacia, and Paget’s disease directly affect bone structure.
- Preventing fractures: Understanding bone’s structural weaknesses can help identify individuals at risk of fractures and implement preventative measures.
- Developing new bone-related therapies: A deeper knowledge of bone biology can lead to the development of more effective treatments for bone disorders.
- Promoting overall health: Bone health is closely linked to overall health, influencing calcium metabolism, hormone regulation, and even immune function.
Introducing the Osteon: The Haversian System
The osteon, or Haversian System, is the primary structural unit of compact bone, the dense outer layer of bone that provides strength and support.
Imagine tiny, weight-bearing pillars aligned along the bone’s axis; these are osteons. Each osteon is a cylindrical structure consisting of concentric layers of bone matrix surrounding a central canal.
Article Purpose: Defining and Exploring the Osteon
This article aims to provide a comprehensive understanding of the osteon, covering its definition, components, and function. We will explore the following aspects:
- Defining the osteon: Providing a clear and concise definition of this fundamental structural unit.
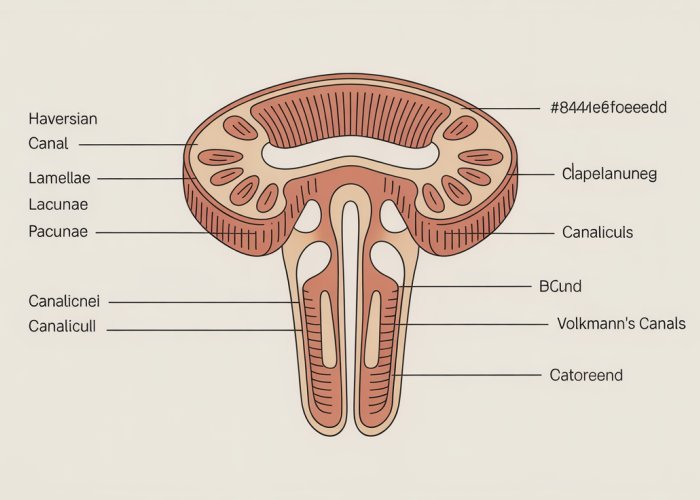
- Anatomy of the osteon: Examining the key components, including the Haversian canal, lamellae, lacunae, and canaliculi.
- Function of the osteon: Understanding the role of the osteon in providing strength, facilitating nutrient exchange, and enabling bone remodeling.
Bone, far from being the static, inert material we often perceive, is a dynamic and complex tissue, constantly adapting and remodeling itself throughout our lives. Understanding its intricate structure is not merely an academic exercise; it’s crucial for comprehending overall health, from preventing fractures to managing metabolic diseases.
At the heart of compact bone lies a remarkable structural unit: the osteon, also known as the Haversian System. This microscopic marvel is the fundamental building block that provides bone with its strength and resilience.
This article embarks on a journey into the microscopic world of bone, with the central aim of providing a comprehensive definition of the osteon and exploring its multifaceted components. By delving into its anatomy and function, we aim to illuminate the vital role it plays in skeletal health.
Bone tissue is continuously undergoing a process of formation and resorption, responding to mechanical stress, hormonal signals, and nutritional factors. This dynamic nature allows bone to adapt to changing demands and repair damage.
The complexity of bone extends to its cellular composition, which includes osteoblasts (bone-forming cells), osteocytes (mature bone cells), and osteoclasts (bone-resorbing cells), all working in concert to maintain skeletal integrity.
A thorough understanding of bone structure is essential for several reasons: Conditions like osteoporosis, osteomalacia, and Paget’s disease directly affect bone structure.
Now that we’ve established the importance of understanding bone architecture and its dynamic nature, let’s turn our attention to the osteon itself. What exactly is this fundamental unit, and why is it so crucial for bone health?
Defining the Osteon: The Haversian System Explained
The osteon, or Haversian System, represents the chief structural unit of compact bone.
It’s a complex, cylindrical arrangement of bone cells and matrix that provides strength and pathways for nutrient exchange.
Osteon: A Precise Definition
In precise terms, an osteon can be defined as a concentric arrangement of lamellae surrounding a central canal, known as the Haversian canal.
These lamellae are essentially layers of bone matrix, the hard, calcified material that gives bone its rigidity.
Think of it as a series of tubes within tubes, each playing a critical role in the bone’s overall integrity.
Haversian System: Another Name for the Osteon
It’s crucial to understand that the terms "osteon" and "Haversian System" are interchangeable.
The term "Haversian System" honors Clopton Havers, the English physician who first described these structures in the 17th century.
Therefore, when you encounter either term, rest assured that they both refer to the same fundamental unit of compact bone.
Location: Exclusively in Compact Bone
Osteons are exclusively found in compact bone, also known as cortical bone.
This type of bone forms the hard, outer layer of most bones in the body.
It’s this compact arrangement of osteons that gives compact bone its characteristic density and strength, enabling it to withstand significant stress and weight-bearing forces.
The Function of Osteons
The primary function of the osteon is to provide a structural framework for compact bone.
By organizing bone matrix into concentric lamellae around a central canal, osteons maximize bone’s resistance to bending and twisting forces.
Furthermore, the Haversian canal within each osteon provides a pathway for blood vessels and nerves to supply bone cells with nutrients and oxygen and remove waste products.
This intricate network ensures the vitality and functionality of bone tissue.
Now that we’ve established the importance of understanding bone architecture and its dynamic nature, let’s turn our attention to the osteon itself. What exactly is this fundamental unit, and why is it so crucial to the integrity of our skeletal system?
Anatomy of an Osteon: A Deep Dive into its Components
The osteon, a cylindrical structure, is a marvel of biological engineering. To truly appreciate its significance, we must dissect its anatomy, examining each component and understanding its specific role.
Haversian Canal: The Central Highway
At the very heart of each osteon lies the Haversian canal, a central channel that runs longitudinally through the bone.
Think of it as the osteon’s lifeline, providing passage for essential elements.
The Haversian canal is not an empty tunnel. It’s a bustling thoroughfare containing vital blood vessels that nourish the bone tissue, and nerves that regulate bone activity and transmit sensory information.
This intricate network ensures that osteocytes, the bone cells, receive the nutrients and signals necessary for their survival and function.
Lamellae: Concentric Layers of Strength
Surrounding the Haversian canal are concentric layers of bone matrix called lamellae.
These are essentially rings of hardened tissue, much like the growth rings of a tree, providing the osteon with its remarkable strength.
Lamellae are not simply uniform layers of bone. They are composed primarily of collagen fibers and hydroxyapatite, a mineral form of calcium phosphate.
Collagen provides flexibility and tensile strength, while hydroxyapatite provides rigidity and compressive strength. This combination gives bone its characteristic resilience.
The arrangement of collagen fibers within each lamella is particularly noteworthy. The fibers are oriented in a specific direction, and the direction changes in adjacent lamellae.
This alternating pattern of collagen orientation provides exceptional resistance to stress and prevents cracks from propagating through the bone.
It’s a clever design that maximizes strength and minimizes the risk of fracture.
Lacunae: Homes for Bone Cells
Scattered between the lamellae are small spaces called lacunae. These are essentially tiny "lakes" within the bone matrix.
Each lacuna houses an osteocyte, a mature bone cell responsible for maintaining the bone matrix.
The osteocytes are the long-term residents of the bone, monitoring its condition and responding to changes in stress or damage.
Canaliculi: Connecting the Network
Radiating from the lacunae are tiny channels called canaliculi, creating a vast, interconnected network throughout the osteon.
These microscopic canals connect the lacunae to each other and, most importantly, to the Haversian canal.
The canaliculi are the key to nutrient exchange and waste removal for the osteocytes.
Because bone matrix is a dense, mineralized tissue, osteocytes cannot directly access nutrients from the blood vessels in the Haversian canal.
Instead, nutrients and oxygen diffuse through the canaliculi, reaching the osteocytes, while waste products are transported away. This intricate communication network is essential for maintaining the health and viability of the bone tissue.
Osteocytes: The Caretakers of Bone
Having explored the intricate architecture of the osteon – the central Haversian canal, the concentric lamellae, and the lacunae that dot this landscape – it’s time to meet the residents of this bony city: the osteocytes. These cells, though seemingly passive, are the linchpins of bone health, orchestrating the ongoing maintenance and remodeling of the bone matrix.
The Osteocyte’s Role in Bone Maintenance
Osteocytes are mature bone cells that reside within the lacunae, those small spaces nestled between the lamellae. These cells are essentially osteoblasts that have become entombed within the very matrix they secreted.
However, their entombment doesn’t equate to inactivity. Instead, osteocytes transform into highly specialized cells responsible for maintaining the integrity of the surrounding bone matrix.
They achieve this through a delicate balance of matrix synthesis and resorption, constantly sensing and responding to changes in mechanical load and metabolic needs. This continuous process is crucial for repairing micro-damage, preserving bone strength, and regulating mineral homeostasis.
In essence, osteocytes act as mechanosensors, detecting mechanical strain and signaling to other bone cells (osteoblasts and osteoclasts) to initiate remodeling processes when needed. This ensures that bone adapts to its environment and remains structurally sound.
Canaliculi: The Intricate Communication Network
While osteocytes reside in individual lacunae, they are not isolated entities. They are interconnected through a vast network of tiny channels called canaliculi.
These canaliculi radiate from each lacuna, creating a complex web that links osteocytes to each other and to the Haversian canal. This network is the lifeline of the osteon, facilitating the transport of nutrients, oxygen, and signaling molecules to the osteocytes, as well as the removal of waste products.
More importantly, the canalicular network provides a means for cell-to-cell communication. Osteocytes extend long, slender processes through the canaliculi, forming gap junctions with neighboring osteocytes.
These gap junctions allow for the direct exchange of ions and small molecules, enabling rapid and coordinated responses to stimuli. Through this intricate communication system, osteocytes can act as a unified network, sensing and responding to changes in the bone microenvironment.
This interconnectedness is paramount for maintaining bone health. Damage or disruption to the canalicular network can impair nutrient supply, hinder waste removal, and disrupt cell signaling, ultimately leading to bone weakening and increased fracture risk.
Therefore, the health and functionality of osteocytes, along with the integrity of the canalicular network, are essential for the overall strength, resilience, and adaptability of bone.
Volkmann’s Canals: Interconnecting the System
The osteon, with its concentric lamellae and central Haversian canal, might seem like a self-contained unit. But these structures don’t exist in isolation. They are part of a larger, interconnected network that ensures the entire bone receives the nutrients and signals it needs. This vital connectivity is provided by Volkmann’s canals, also known as perforating canals.
Defining Volkmann’s Canals
Volkmann’s canals are channels that run perpendicular to the Haversian canals, penetrating the compact bone. Unlike Haversian canals, they are not surrounded by concentric lamellae. Think of them as essential connectors that weave through the bone matrix, linking the individual osteons.
The Role of Interconnection
The primary function of Volkmann’s canals is to create a cohesive vascular network within the bone. They act as conduits, connecting Haversian canals to each other.
This interconnection allows blood vessels and nerves to travel between adjacent osteons. This guarantees that all bone cells, regardless of their location within the compact bone, receive adequate nourishment and can effectively communicate.
Volkmann’s canals also extend to the outer and inner surfaces of the bone, connecting the Haversian canals to the periosteum (the outer membrane of the bone) and the endosteum (the inner lining of the bone).
This connection is critical because it facilitates the exchange of nutrients and waste products between the bone tissue and the broader circulatory system. It also allows for communication between bone cells and cells in the periosteum and endosteum, which are involved in bone growth and repair.
A Unified Vascular Network
The intricate network formed by Volkmann’s canals is essential for maintaining bone health. By connecting Haversian canals, the periosteum, and the endosteum, they ensure that nutrients are distributed evenly throughout the bone tissue.
This unified vascular network allows for efficient delivery of oxygen and essential minerals.
It also promotes the removal of waste products, preventing the buildup of toxins that could damage bone cells. Ultimately, the existence of Volkmann’s canals emphasizes the importance of bone as a living, dynamic tissue that requires constant communication and nourishment.
Volkmann’s canals, therefore, are more than just anatomical features; they are crucial for the bone’s survival, enabling a continuous flow of resources and communication that is essential for its function. But bone is not a static structure. It is a living tissue that constantly adapts and renews itself through a process called remodeling.
Bone Remodeling: The Osteon’s Dynamic Life Cycle
Bone remodeling is a continuous process of bone resorption (breakdown) and bone formation, orchestrated by specialized cells that work in a coordinated manner. This dynamic process allows bone to adapt to mechanical stress, repair damage, and maintain mineral homeostasis.
It also ensures the removal of older, potentially weakened bone and its replacement with new, stronger tissue. This constant turnover is particularly evident at the level of the osteon, where existing structures are continually being reshaped and replaced.
The Bone Remodeling Unit (BRU)
The cellular basis of bone remodeling is the Bone Remodeling Unit (BRU), a transient anatomical structure composed of osteoclasts and osteoblasts.
Osteoclasts are responsible for bone resorption, while osteoblasts are responsible for bone formation.
The BRU moves through the bone matrix, creating new osteons in its wake.
This process is tightly regulated by various factors, including hormones, growth factors, and mechanical loading.
Stages of Bone Remodeling
Bone remodeling occurs in a series of coordinated steps:
- Activation: The process begins with the activation of osteoclasts, which are recruited to the site of remodeling.
- Resorption: Osteoclasts then resorb bone, creating a cavity known as a resorption bay.
- Reversal: Following resorption, there is a reversal phase where mononuclear cells prepare the bone surface for new bone formation.
- Formation: Osteoblasts are then recruited to the site and begin to deposit new bone matrix, gradually filling in the resorption bay.
- Quiescence: Finally, the newly formed bone undergoes a period of quiescence, where it is remodeled and mineralized.
Osteon Adaptation to Stress
The structure of the osteon is not fixed; it is adaptable and can change over time in response to mechanical stress.
When bone is subjected to increased stress, such as during exercise, osteoblasts are stimulated to deposit more bone matrix, resulting in thicker and stronger osteons.
Conversely, when bone is subjected to decreased stress, such as during prolonged bed rest, osteoclasts resorb bone, leading to thinner and weaker osteons.
This ability to adapt to stress is crucial for maintaining bone strength and preventing fractures.
The orientation of osteons also aligns with the direction of the principal stresses acting on the bone, maximizing its resistance to bending and torsion.
Age-Related Changes in Osteon Structure
As we age, the rate of bone remodeling decreases, and the balance between bone resorption and bone formation shifts towards resorption.
This leads to a gradual loss of bone mass and a weakening of the skeleton, increasing the risk of fractures.
The structure of osteons also changes with age.
The number of osteons decreases, and the size of Haversian canals increases.
These changes compromise the mechanical integrity of bone and contribute to age-related bone loss.
Bone Remodeling and Disease
Various diseases can disrupt the normal process of bone remodeling, leading to abnormal bone structure and function.
For example, in osteoporosis, bone resorption exceeds bone formation, resulting in a decrease in bone density and an increased risk of fractures.
In Paget’s disease, bone remodeling is accelerated and disorganized, leading to the formation of abnormally shaped and weakened bones.
Understanding the role of bone remodeling in health and disease is essential for developing effective strategies to prevent and treat bone disorders.
Bone remodeling ensures that our skeletons are not static, unchanging structures. This process allows bones to heal from injury, adapt to changing physical demands, and maintain the mineral balance necessary for overall health. But beyond the cellular mechanisms and hormonal controls, how does the microscopic architecture of the osteon contribute to the bigger picture of bone health?
Osteon Structure and Bone Health: A Critical Connection
The osteon, with its intricate arrangement of lamellae, lacunae, and canaliculi, isn’t just a pretty microscopic picture. It’s a fundamental determinant of bone’s strength and ability to withstand stress. The architecture of the osteon is crucial for understanding the bigger picture of bone health.
Osteon Architecture: The Foundation of Bone Strength
The concentric lamellar arrangement within an osteon provides exceptional resistance to compressive forces. Think of it like a series of nested cylinders, each layer reinforcing the next.
The collagen fibers within each lamella are oriented in different directions, further enhancing the bone’s ability to withstand stress from multiple angles. This arrangement distributes stress.
The Haversian canal at the center provides essential nutrients to osteocytes, ensuring their viability and their ability to maintain the bone matrix.
When the osteon’s structure is compromised, the entire bone’s integrity is at risk.
Factors Affecting Osteon Structure and Bone Health
Several factors can disrupt the delicate balance of osteon formation and remodeling, leading to weakened bones.
Age-Related Changes
As we age, the rate of bone remodeling slows down. This can lead to a decrease in the number of osteons and an increase in the number of incomplete or fragmented osteons.
The result is a gradual decline in bone density and increased susceptibility to fractures, a hallmark of osteoporosis.
Nutritional Deficiencies
Calcium and vitamin D are critical for bone health, and their deficiency can directly impact osteon structure. Calcium is, of course, the primary building block.
Vitamin D is essential for calcium absorption. Lack of these nutrients can lead to poorly mineralized osteons. This results in weaker, more brittle bones.
Diseases and Medications
Certain diseases, such as hyperparathyroidism, can accelerate bone remodeling, leading to an imbalance between bone resorption and formation.
This can result in the formation of structurally unsound osteons.
Some medications, like long-term corticosteroid use, can also negatively affect osteon structure and bone health.
The Impact of Mechanical Loading
Wolff’s Law states that bone adapts to the stresses placed upon it. Regular weight-bearing exercise stimulates bone formation and strengthens osteons.
Conversely, a sedentary lifestyle can lead to decreased bone density and weaker osteons.
This highlights the importance of physical activity in maintaining skeletal health throughout life.
Osteon FAQs: Understanding Bone’s Building Blocks
What is the primary function of an osteon in bone?
The main function of an osteon, also known as a Haversian system, is to provide a pathway for blood vessels and nerves to travel through the dense, compact bone tissue. This ensures the bone cells receive necessary nutrients and can communicate with the body. Essentially, osteons facilitate bone maintenance and repair.
How does the definition of osteon relate to bone strength?
The definition of osteon is intrinsically tied to bone strength. Osteons, with their concentric lamellae arranged around a central canal, create a strong, weight-bearing structure. The cylindrical shape resists bending and twisting forces, contributing significantly to overall bone integrity and resistance to fractures.
What are the main components of an osteon?
The major components include the Haversian canal (containing blood vessels and nerves), concentric lamellae (layers of bone matrix), lacunae (small spaces housing osteocytes), and canaliculi (tiny channels connecting lacunae). These components work together to form a functional unit crucial for bone health.
How do osteons differ in compact bone versus spongy bone?
Osteons are the fundamental structural unit of compact bone, providing its density and strength. Spongy bone, also known as cancellous bone, does not contain true osteons. Instead, it consists of a network of trabeculae, which are irregularly arranged plates of bone tissue. These trabeculae receive nutrients directly from the marrow spaces.
Hopefully, this gave you a solid understanding of the definition of osteon! Now you’re ready to impress your friends (or ace that exam!). Best of luck continuing your learning journey!