Optical Coherence Tomography, or OCT, plays a crucial role in the diagnosis and management of various retinal conditions. Subretinal Fluid (SRF), often visualized through OCT imaging, is a key indicator in conditions like Central Serous Chorioretinopathy (CSC). Understanding the characteristics of oct subretinal fluid is essential for effective treatment planning by retinal specialists. Research institutions, such as The National Eye Institute (NEI), continue to advance our knowledge of the underlying mechanisms and novel therapeutic approaches for managing oct subretinal fluid.
Understanding OCT Subretinal Fluid: Causes, Diagnosis, and Modern Treatments
This document provides a comprehensive overview of subretinal fluid (SRF) as detected by Optical Coherence Tomography (OCT), commonly referred to as "OCT subretinal fluid". It will explore the underlying causes of this fluid accumulation, the diagnostic methods used to identify it, and the current landscape of treatment options.
What is Subretinal Fluid (SRF)?
Subretinal fluid, as the name suggests, is the accumulation of fluid in the space between the neurosensory retina and the retinal pigment epithelium (RPE). The neurosensory retina is the layer of the eye that contains photoreceptor cells responsible for vision, while the RPE is a layer of cells providing nourishment and support to the retina.
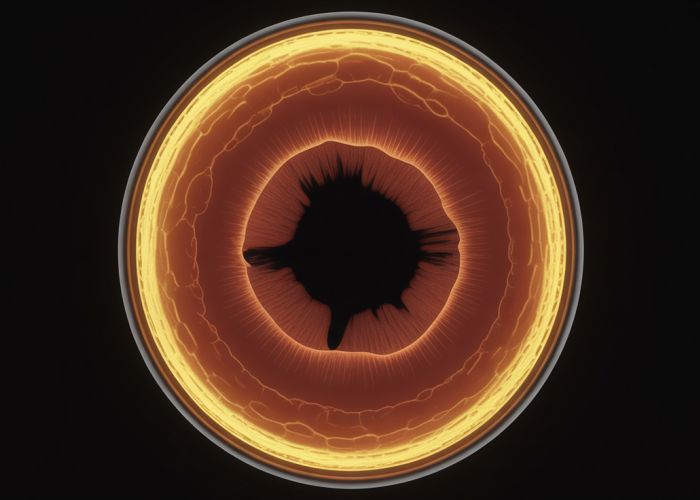
- Visualizing SRF with OCT: OCT is a non-invasive imaging technique that uses light waves to create high-resolution cross-sectional images of the retina. It’s the gold standard for detecting and quantifying SRF. On an OCT scan, SRF typically appears as a hyporeflective (dark) space separating the retina from the RPE.
Causes of OCT Subretinal Fluid
Several conditions can lead to the development of OCT subretinal fluid. Understanding the underlying cause is crucial for effective management.
Common Causes
-
Age-Related Macular Degeneration (AMD):
- Neovascular AMD (Wet AMD): This is a leading cause of SRF. Abnormal blood vessels (choroidal neovascularization or CNV) grow beneath the retina, leaking fluid and blood into the subretinal space.
- Serous Detachment of the RPE: In some cases of AMD, SRF may be related to a serous detachment of the RPE without active neovascularization.
-
Central Serous Chorioretinopathy (CSCR): This condition typically affects younger to middle-aged individuals and is characterized by leakage from the choroid (the vascular layer of the eye) into the subretinal space. Stress, steroid use, and certain personality types have been linked to CSCR.
-
Choroidal Neovascularization (CNV): As mentioned in AMD, CNV from other causes, like myopic degeneration or angioid streaks, can also cause SRF.
-
Retinal Detachment: In rhegmatogenous retinal detachment (where there is a tear or break in the retina), SRF accumulates as fluid seeps through the retinal break and into the subretinal space.
-
Inflammatory Conditions: Uveitis (inflammation of the eye) and other inflammatory conditions can cause vascular leakage and SRF.
-
Other Causes:
- Tumors: Choroidal tumors can disrupt the RPE barrier, leading to SRF.
- Vascular Abnormalities: Conditions like polypoidal choroidal vasculopathy (PCV) can also cause SRF.
- Optic Pit: A congenital cavitary defect in the optic disc occasionally associated with serous macular detachment and SRF.
Less Common Causes
The following table outlines some less prevalent conditions that can cause subretinal fluid:
| Cause | Description |
|---|---|
| Harada’s Disease | An autoimmune disease causing inflammation of the choroid and retina, often leading to serous retinal detachment. |
| Posterior Scleritis | Inflammation of the sclera (the white part of the eye) that can extend to the choroid. |
| Nanophthalmos | A rare condition characterized by abnormally small eyes, which can predispose individuals to SRF. |
| Drug-Induced Causes | Certain medications, such as corticosteroids, have been implicated in SRF development. |
Diagnosis of OCT Subretinal Fluid
The diagnostic process involves a comprehensive eye examination and various imaging techniques.
-
Clinical Examination: A thorough eye examination, including dilated fundus examination, is essential to assess the overall health of the retina and choroid.
-
Optical Coherence Tomography (OCT): As mentioned earlier, OCT is crucial for detecting and quantifying SRF. It can also help differentiate between different types of SRF and identify associated features like retinal thickening or intraretinal fluid.
-
Fluorescein Angiography (FA): This imaging technique involves injecting a dye (fluorescein) into the bloodstream and taking pictures of the retinal blood vessels. FA can help identify areas of leakage or neovascularization, particularly in cases of wet AMD or CNV.
-
Indocyanine Green Angiography (ICGA): Similar to FA, ICGA uses a different dye (indocyanine green) that better visualizes the choroidal vasculature. This is especially helpful in diagnosing conditions like PCV.
-
Other Imaging Modalities: In certain cases, other imaging modalities like fundus autofluorescence (FAF) or enhanced depth imaging OCT (EDI-OCT) may be used to further characterize the underlying pathology.
Treatment Options for OCT Subretinal Fluid
The treatment approach for OCT subretinal fluid depends entirely on the underlying cause.
Treatment Strategies for Common Causes
-
Wet AMD:
- Anti-VEGF Injections: These medications (e.g., ranibizumab, aflibercept, brolucizumab) inhibit the growth of abnormal blood vessels and reduce leakage, leading to SRF resolution. They are injected directly into the vitreous cavity of the eye.
- Photodynamic Therapy (PDT): In some cases, PDT may be used in conjunction with anti-VEGF injections. PDT involves injecting a light-sensitive drug (verteporfin) into the bloodstream and then using a non-thermal laser to activate the drug, which damages the abnormal blood vessels.
-
Central Serous Chorioretinopathy (CSCR):
- Observation: In many cases, CSCR resolves spontaneously without treatment.
- Laser Photocoagulation: This involves using a laser to seal the leakage point in the choroid. It is typically reserved for chronic or recurrent cases.
- Half-Dose Photodynamic Therapy (PDT): Half-dose PDT is often considered as a preferred treatment over conventional laser for CSCR due to lower risk of complications.
- Mineralocorticoid Receptor Antagonists: Medications like eplerenone have shown promise in reducing SRF in CSCR by targeting the mineralocorticoid receptor pathway.
-
Retinal Detachment:
- Surgery: Surgical repair is necessary to reattach the retina and eliminate the SRF. Common surgical techniques include pneumatic retinopexy, scleral buckle, and vitrectomy.
-
Inflammatory Conditions:
- Corticosteroids: Oral or topical corticosteroids may be used to reduce inflammation and vascular leakage.
- Immunosuppressants: In more severe cases, immunosuppressant medications may be necessary to control the inflammation.
-
Other Treatments: Treatment of the primary cause such as removing a choroidal tumor or correcting a vascular anomaly.
OCT Subretinal Fluid: Frequently Asked Questions
Here are some common questions about subretinal fluid detected through OCT imaging, its causes, and the latest treatment options.
What exactly is subretinal fluid?
Subretinal fluid (SRF) refers to fluid that accumulates between the neurosensory retina and the retinal pigment epithelium (RPE). It’s often identified during an OCT (Optical Coherence Tomography) scan of the eye. The presence of oct subretinal fluid can indicate various underlying retinal conditions.
What are common causes of oct subretinal fluid?
Common causes include age-related macular degeneration (AMD), central serous chorioretinopathy (CSC), retinal vein occlusions, and inflammatory conditions. Sometimes, other issues like choroidal neovascularization can lead to the presence of oct subretinal fluid. Your ophthalmologist will need to diagnose the underlying cause.
How is subretinal fluid detected?
Subretinal fluid is primarily detected through Optical Coherence Tomography (OCT). This non-invasive imaging technique provides detailed cross-sectional images of the retina, allowing doctors to visualize and quantify any fluid accumulation. Regular OCT scans are crucial for monitoring the progression of conditions associated with oct subretinal fluid.
What are the latest treatments for subretinal fluid?
Treatment depends on the underlying cause. Anti-VEGF injections are commonly used for AMD. Laser photocoagulation or photodynamic therapy (PDT) may be used for CSC. Managing the underlying condition often leads to the resolution of oct subretinal fluid. Your doctor will determine the most appropriate course of treatment based on your individual diagnosis.
So, that’s the scoop on oct subretinal fluid! Hopefully, you found this helpful. If you’re dealing with any eye issues, definitely chat with your doctor. Best of luck with your eye health!