The intricate process of human reproduction hinges significantly on the male gamete name. Spermatogenesis, a crucial biological mechanism, ensures the continuous production of these essential cells within the testes. A deeper understanding of male gamete name requires examining its motility, which is vital for successful fertilization; WHO (World Health Organization) guidelines provide crucial parameters for assessing sperm quality. Furthermore, research conducted at the American Society for Reproductive Medicine (ASRM) highlights advanced techniques for analyzing male gamete name morphology, enabling improved diagnostic capabilities in fertility treatments. The journey of these cells is fundamental to life itself.
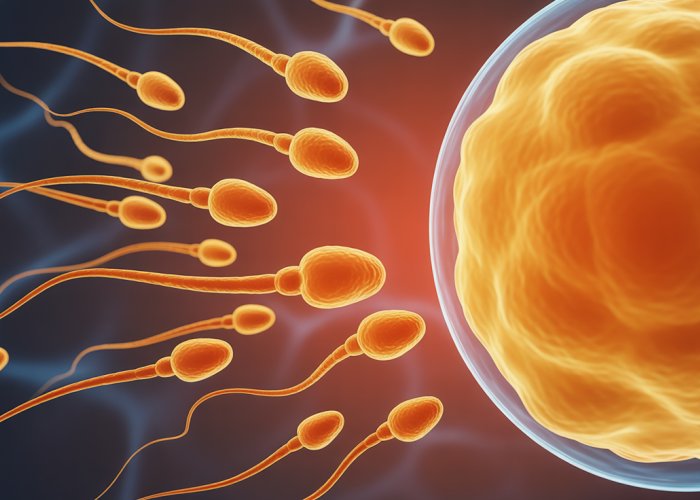
At the heart of sexual reproduction lies a fundamental question: How do two distinct organisms combine their genetic material to create a new, unique individual? The answer, in the case of males, resides within a single, remarkably specialized cell: the sperm.
This microscopic entity, also known as a spermatozoon, is far more than just a vessel for DNA. It’s a meticulously engineered vehicle designed for a singular, crucial purpose: to navigate the complex landscape of the female reproductive tract and deliver its precious cargo to the awaiting egg.
Unveiling the Secrets of the Sperm Cell
This blog post is dedicated to providing a comprehensive exploration of the sperm cell. We aim to dissect its intricate anatomy, understand its complex functions, and appreciate its profound significance in the grand scheme of life.
A Journey Begins
Imagine a cell so small it’s practically invisible to the naked eye, yet possesses the power to initiate the creation of an entirely new being. This is the reality of the sperm cell.
But there is more than meets the eye.
It’s a testament to biological engineering. A marvel of natural selection. A key player in the ongoing drama of evolution. Join us as we delve into the astonishing world of the male gamete and uncover the secrets hidden within.
At the heart of sexual reproduction lies a fundamental question: How do two distinct organisms combine their genetic material to create a new, unique individual? The answer, in the case of males, resides within a single, remarkably specialized cell: the sperm.
This microscopic entity, also known as a spermatozoon, is far more than just a vessel for DNA. It’s a meticulously engineered vehicle designed for a singular, crucial purpose: to navigate the complex landscape of the female reproductive tract and deliver its precious cargo to the awaiting egg.
Having set the stage with an appreciation for the sperm cell’s critical role, let’s delve into the specifics of its form and function. Understanding its anatomy, alongside the composition of semen and the functionality of the testes, is essential to grasping the intricacies of male reproduction.
Decoding the Sperm Cell: Anatomy and Function
The journey to understanding the sperm cell begins with a detailed examination of its architecture. This seemingly simple cell is a marvel of biological engineering, perfectly designed for its mission.
The Sperm Cell (Spermatozoon): Structure and Purpose
The sperm cell, or spermatozoon, is composed of three primary parts: the head, the midpiece, and the tail. Each section plays a vital role in the sperm’s journey to fertilization.
-
The Head: This oval-shaped structure houses the genetic material (DNA) in the nucleus. The acrosome, a cap-like structure covering the anterior portion of the head, contains enzymes essential for penetrating the outer layers of the egg.
-
The Midpiece: Acting as the engine room, the midpiece is packed with mitochondria. These organelles generate the energy (ATP) required for the sperm’s motility.
-
The Tail (Flagellum): The tail, or flagellum, is a long, whip-like appendage that propels the sperm forward. Its movement is crucial for navigating the female reproductive tract.
Semen: The Sperm’s Life Support System
Sperm cells don’t travel alone. They are suspended in semen, a complex fluid that provides them with the necessary support and protection.
Semen is more than just a transport medium. It’s a carefully crafted concoction with several critical components:
-
Seminal Fluid: This fluid, primarily produced by the seminal vesicles, provides a fructose-rich energy source for the sperm. It also contains substances that help neutralize the acidic environment of the female reproductive tract.
-
Enzymes: Semen contains various enzymes that aid in liquefying the ejaculate, allowing the sperm to move more freely.
-
Nutrients and Buffers: These components provide essential nutrients and help maintain an optimal pH balance for sperm survival and motility.
Testes (Testicles): The Sperm Production Factory
The testes, or testicles, are the primary male reproductive organs responsible for sperm production (spermatogenesis). They are located within the scrotum, a sac-like structure that hangs outside the body to maintain a slightly lower temperature than the core body temperature, which is optimal for sperm development.
The testes are complex organs with several key features:
-
Seminiferous Tubules: These are the sites of spermatogenesis. Within these tubules, specialized cells undergo a series of divisions and transformations to become mature sperm cells.
-
Sertoli Cells: These "nurse" cells support and nourish developing sperm cells within the seminiferous tubules.
-
Leydig Cells: Located in the interstitial tissue surrounding the seminiferous tubules, Leydig cells produce testosterone. This hormone is crucial for the development and maintenance of male characteristics, as well as for spermatogenesis.
The interplay between the structure of the sperm cell, the composition of semen, and the function of the testes is a testament to the intricate design of the male reproductive system. Each component plays a critical role in the journey towards fertilization and the continuation of life.
At the heart of understanding the sperm cell lies not only its individual structure and function, but also the incredible journey it undertakes. From its very genesis to the moment of conception, the sperm’s path is fraught with challenges, a testament to the intricate orchestration of biological processes that govern reproduction.
The Sperm’s Odyssey: A Journey to Fertilization
The sperm cell’s existence is defined by a singular, relentless purpose: to deliver its genetic payload to the egg. This section navigates the epic voyage of the sperm, from its intricate creation within the testes to its ultimate triumph – the fusion of genetic material in fertilization.
Spermatogenesis: The Genesis of a Sperm Cell
Spermatogenesis is the highly regulated process through which spermatogonia, the primitive germ cells, transform into mature spermatozoa. This complex transformation unfolds within the seminiferous tubules of the testes and is orchestrated by a symphony of hormonal signals.
Stages of Spermatogenesis
The process can be divided into three major stages: mitosis, meiosis, and spermiogenesis.
-
Mitosis: Spermatogonia undergo mitotic divisions to produce a larger pool of cells, some of which differentiate into primary spermatocytes.
-
Meiosis: Primary spermatocytes undergo meiosis I and meiosis II, resulting in haploid spermatids. This reduction division is crucial to ensure that the offspring receives the correct number of chromosomes.
-
Spermiogenesis: Spermatids undergo a dramatic morphological transformation, developing a flagellum (tail), condensing their DNA, and forming an acrosome. The acrosome is crucial for fertilization.
Hormonal Regulation of Spermatogenesis
The entire process is tightly controlled by hormones, primarily testosterone and follicle-stimulating hormone (FSH). Testosterone, produced by Leydig cells in the testes, is essential for spermatogenesis and the development of male secondary sexual characteristics. FSH stimulates Sertoli cells, which support and nourish the developing sperm cells.
Epididymis: Maturation and Storage
Once spermatogenesis is complete, the newly formed spermatozoa are released into the epididymis. This coiled tube, adjacent to the testis, serves as a crucial site for sperm storage and maturation.
Within the epididymis, sperm undergo further biochemical and physiological changes, acquiring the capacity for motility. This maturation process is essential for the sperm to effectively navigate the female reproductive tract and fertilize the egg.
The epididymis also acts as a reservoir, storing mature sperm until ejaculation.
DNA and Chromosomes: The Genetic Blueprint
The sperm cell is the carrier of the male genetic contribution. Its nucleus contains tightly packed DNA organized into chromosomes. Human sperm cells carry 23 chromosomes, half the number found in somatic cells.
Gender Determination
One of the 23 chromosomes is a sex chromosome, either an X or a Y. If the sperm carries an X chromosome, fertilization will result in a female (XX) offspring. If it carries a Y chromosome, the offspring will be male (XY). This simple genetic mechanism determines the sex of the offspring.
Importance of DNA Integrity
The integrity of sperm DNA is paramount for successful fertilization and healthy embryo development. DNA damage, such as fragmentation or mutations, can lead to infertility, miscarriage, or developmental abnormalities.
Factors such as oxidative stress, exposure to toxins, and infection can all compromise sperm DNA integrity.
Fertilization: The Ultimate Goal
The journey culminates in fertilization, the fusion of the sperm and egg, initiating the development of a new individual. This is a highly coordinated process involving a series of crucial steps.
Sperm Capacitation
Before fertilization can occur, sperm must undergo capacitation within the female reproductive tract. This physiological process involves changes to the sperm’s plasma membrane, preparing it to undergo the acrosome reaction.
The Acrosome Reaction
Upon contacting the egg’s outer layer (zona pellucida), the sperm undergoes the acrosome reaction. This involves the release of enzymes from the acrosome, enabling the sperm to penetrate the zona pellucida and reach the egg’s plasma membrane.
Fusion and Genetic Union
Once the sperm penetrates the egg, the plasma membranes of the two cells fuse. The sperm’s nucleus then enters the egg’s cytoplasm, and the genetic material from both the sperm and egg combine to form a zygote, the first cell of the new organism. This remarkable union marks the beginning of a new life.
The sperm’s journey is a carefully orchestrated event, but successful fertilization is not solely reliant on the initial launch. The health and vitality of the sperm themselves play an indispensable role in determining reproductive success. The parameters of sperm health, specifically count, motility, and morphology, are critically intertwined with a couple’s ability to conceive.
Sperm Health: Quality, Quantity, and Reproductive Success
The ability of sperm to successfully navigate the female reproductive tract, penetrate the egg, and deliver its genetic cargo is directly linked to its health. Healthy sperm parameters—count, motility, and morphology—are paramount for successful reproduction. When these parameters fall outside of the normal ranges, the likelihood of conception decreases, highlighting the importance of understanding and optimizing sperm health.
The Pillars of Sperm Health: Count, Motility, and Morphology
A comprehensive assessment of sperm health considers three key factors: sperm count, motility, and morphology. Each plays a unique and vital role in the fertilization process.
-
Sperm Count: Refers to the concentration of sperm in a semen sample. A sufficient number of sperm is necessary to increase the odds of at least one sperm successfully reaching and fertilizing the egg.
-
Motility: Describes the sperm’s ability to move efficiently. Progressive motility, the ability to swim in a straight line, is particularly crucial for navigating the female reproductive tract.
-
Morphology: Refers to the sperm’s shape and structure. Sperm with a normal shape are more likely to be able to penetrate the egg.
Factors Undermining Sperm Health: A Multifaceted Threat
Numerous factors can negatively impact sperm health, influencing count, motility, and morphology. These influences can be broadly categorized into lifestyle, environmental, and medical factors. Understanding these threats is the first step in mitigating their impact.
Lifestyle Choices: Diet, Exercise, and Vices
Lifestyle choices exert a considerable influence on sperm health. A balanced diet rich in antioxidants, vitamins, and minerals is essential for optimal sperm production. Conversely, processed foods, excessive sugar intake, and nutrient deficiencies can impair sperm quality.
Regular exercise promotes healthy hormone levels and circulation, both of which are beneficial for sperm production. However, excessive or intense exercise can sometimes have a negative impact.
Smoking and excessive alcohol consumption are well-established risk factors for impaired sperm health. Nicotine and alcohol can damage sperm DNA, reduce sperm count, and decrease motility.
Environmental Exposure: Toxins and Heat
Exposure to environmental toxins can have detrimental effects on sperm health. Pesticides, heavy metals, and industrial chemicals have all been linked to decreased sperm quality.
Elevated testicular temperature can also impair sperm production. Prolonged exposure to heat sources, such as hot tubs, saunas, and tight-fitting clothing, should be avoided. Certain occupations involving prolonged sitting or heat exposure may also pose a risk.
Medical Conditions: Varicocele and Infections
Certain medical conditions can directly impact sperm production and quality. Varicocele, an enlargement of the veins within the scrotum, can increase testicular temperature and impair sperm development.
Infections, such as sexually transmitted infections (STIs), can damage the reproductive organs and lead to inflammation, affecting sperm production and motility. Hormonal imbalances can also disrupt spermatogenesis.
Navigating Male Infertility: Seeking Expert Guidance
When conception proves challenging, it’s essential to consider the possibility of male infertility. Several conditions can contribute to male infertility, and seeking professional help is paramount for accurate diagnosis and effective management.
Common Causes of Male Infertility: Azoospermia to Teratozoospermia
-
Azoospermia: Complete absence of sperm in the ejaculate.
-
Oligozoospermia: Low sperm count.
-
Asthenozoospermia: Reduced sperm motility.
-
Teratozoospermia: Abnormal sperm morphology.
These conditions can arise from a variety of factors, including genetic abnormalities, hormonal imbalances, blockages in the reproductive tract, or the factors affecting sperm health previously discussed.
The Role of Urologists and Andrologists
Urologists and andrologists are specialists in male reproductive health. They can diagnose the underlying causes of male infertility through a thorough evaluation, including semen analysis, physical examination, and hormonal testing.
Based on the diagnosis, these specialists can recommend appropriate treatment options, which may include lifestyle modifications, medications, surgery, or assisted reproductive technologies (ART) such as in-vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI).
The journey into understanding sperm health and its impact on reproductive success reveals a complex and often misunderstood landscape. Before we continue, let’s tackle the common misconceptions that surround this crucial aspect of human biology.
Sperm Myths and Facts: Separating Truth from Fiction
The world of sperm, male fertility, and reproductive health is often shrouded in misconceptions and old wives’ tales. Separating fact from fiction is crucial for informed decision-making and a clearer understanding of male reproductive potential. Let’s debunk some prevalent myths and explore some fascinating truths about sperm.
Debunking Common Myths About Sperm
It is essential to challenge unfounded beliefs with scientific evidence, improving understanding and allaying unnecessary anxiety.
The Myth of Inexhaustible Sperm Count
One pervasive myth is that men have an inexhaustible supply of sperm. While the testes continuously produce sperm, the count and quality can fluctuate due to various factors.
Age, lifestyle, environmental toxins, and underlying medical conditions can all impact sperm production. It’s crucial to understand that sperm production is not infinite.
Sperm Lifespan: Beyond the Immediate
Another common misconception revolves around sperm lifespan. It is often believed that sperm survive only for a very short time after ejaculation.
While sperm can only survive for a few minutes exposed to air, inside the female reproductive tract, they can survive for up to five days, waiting for an egg to be fertilized.
This extended lifespan within the female body is crucial for conception, allowing a window of opportunity even if intercourse doesn’t occur precisely at the moment of ovulation.
Factors Influencing Sperm Production: More Than Just Diet
Many believe that simple dietary changes can drastically improve sperm production. While nutrition plays a role, it’s not the only determinant.
While a healthy diet rich in antioxidants, vitamins, and minerals is beneficial, complex factors such as hormonal balance, genetics, and overall health are also significant.
Unveiling Intriguing Facts About Sperm
Beyond debunking myths, there are fascinating and often surprising facts about sperm that highlight the complexity and wonder of reproductive biology.
The Reality of Sperm Competition
Sperm competition is a real phenomenon in the animal kingdom, and some research suggests it may play a subtle role in humans as well.
Sperm competition refers to the idea that sperm from different males compete to fertilize the egg. Factors such as sperm quantity, motility, and even seminal fluid composition can influence the outcome.
Sperm Speed: The Great Race
The perception of sperm swimming frantically toward the egg is often exaggerated. In reality, sperm speed varies significantly.
Sperm speed is influenced by factors such as viscosity of the semen, the health of the sperm, and the environment of the female reproductive tract. The journey is less about speed and more about endurance and navigation.
Variations in Sperm Morphology
Sperm morphology, or shape, is another area of interest. While "normal" sperm morphology is desired, variations are common.
The definition of "normal" has become more refined over time. Not all sperm need to be perfectly shaped to achieve fertilization. A certain percentage of normal forms is sufficient.
FAQs: Decoding the Male Gamete Name
Here are some frequently asked questions to further clarify the world of male gametes and their names.
What exactly is the male gamete name?
The male gamete name is, quite simply, sperm. It’s the reproductive cell in males responsible for fertilizing the female egg and initiating the creation of a new organism.
Are there any other terms used interchangeably with the male gamete name?
While "sperm" is the most common term, you might occasionally encounter "spermatozoon" or "spermatozoa" (plural). These terms are more scientific but refer to the same thing: the male reproductive cell.
What makes the male gamete, the sperm, so important?
The sperm’s crucial role is to carry the male’s genetic information to the egg. Without this successful fusion, fertilization cannot occur, and a new offspring cannot be created. The male gamete name is therefore synonymous with reproduction itself.
Where are sperm, the male gamete, produced?
Sperm are produced within the testes, specifically in the seminiferous tubules. This process, called spermatogenesis, is ongoing throughout a male’s reproductive years, allowing for continuous production of the male gamete.
So, there you have it! Hopefully, now you have a much clearer idea of what male gamete name is all about. Go forth and impress your friends with your newfound knowledge!