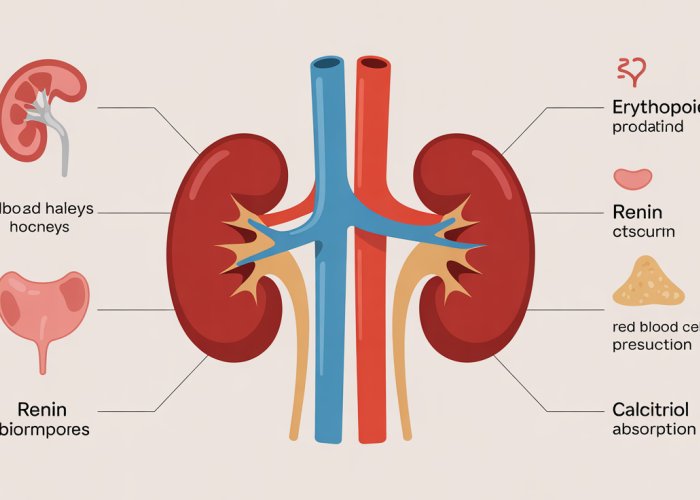
The delicate equilibrium within the human body relies on the intricate communication network orchestrated by hormones of kidney. Erythropoietin (EPO), a vital hormone, promotes red blood cell production, showcasing the kidney’s significant role in hematopoiesis. Vitamin D activation, crucial for calcium absorption and bone health, is another key function mediated by the kidneys, highlighting their involvement in skeletal integrity. The Renin-Angiotensin-Aldosterone System (RAAS), a complex hormonal cascade, depends on renin released by the kidneys to regulate blood pressure and electrolyte balance. Finally, understanding the kidney’s interaction with the adrenal glands, particularly regarding aldosterone secretion, provides a complete picture of the kidney’s broader hormonal influence on homeostasis.
Did you know that approximately 10% of the world’s adult population suffers from chronic kidney disease (CKD)? This staggering statistic underscores the critical importance of understanding these vital organs and their multifaceted roles.
Far too often, the kidneys are simply perceived as filters, quietly removing waste from our blood. While this function is undeniably crucial, it represents only a fraction of their overall contribution to our health.
The Kidney: An Overlooked Endocrine Powerhouse
The kidneys are, in fact, active participants in the endocrine system, a network of glands that produce and release hormones to regulate various bodily functions. These hormones act as messengers, orchestrating processes that extend far beyond simple waste removal.
They play key roles in everything from red blood cell production to blood pressure regulation and calcium homeostasis.
The Hormonal Symphony: A Thesis
This exploration aims to illuminate the often-overlooked hormonal functions of the kidneys, revealing their profound influence on our overall well-being. We will uncover how these potent chemical messengers maintain the delicate balance essential for life, and the consequences that arise when this balance is disrupted.
Did you know that approximately 10% of the world’s adult population suffers from chronic kidney disease (CKD)? This staggering statistic underscores the critical importance of understanding these vital organs and their multifaceted roles.
Far too often, the kidneys are simply perceived as filters, quietly removing waste from our blood. While this function is undeniably crucial, it represents only a fraction of their overall contribution to our health.
As we’ve seen, the kidneys play a far more dynamic role than simply sifting through bodily fluids. They’re not merely passive custodians of our internal environment; they actively shape it. This next section delves into how we must begin to consider the kidneys differently, recognizing them as key players in the endocrine system.
The Kidney: More Than Just a Filter – An Endocrine Powerhouse
For too long, the humble kidney has been relegated to a supporting role in the theater of human physiology. Textbooks often depict them as sophisticated filtration systems, meticulously removing waste products and excess fluids from the bloodstream.
While this portrayal is accurate to a point, it drastically underestimates the kidney’s true potential and its significance in maintaining overall health. It’s time we challenge this limited view and recognize the kidney for what it truly is: an endocrine powerhouse.
Challenging the Conventional View
The pervasive image of the kidney as a mere filtration unit overshadows its diverse and crucial hormonal functions. This narrow perspective stems, in part, from the more obvious and readily measurable aspects of renal function, such as glomerular filtration rate and urine output.
However, focusing solely on these metrics obscures the intricate network of hormonal signals emanating from the kidneys, which influence everything from red blood cell production to blood pressure regulation and bone health.
We must actively dismantle this simplistic understanding and embrace a more holistic view of the kidney as a vital endocrine organ.
The Kidney’s Endocrine Role: An Active Participant
Beyond their well-known excretory functions, the kidneys are, in fact, active participants in the endocrine system, a complex network of glands that produce and release hormones to regulate various bodily functions.
These hormones act as chemical messengers, orchestrating a symphony of physiological processes that extend far beyond waste removal.
The kidneys synthesize and secrete several critical hormones, including erythropoietin (EPO), renin, and calcitriol (the active form of Vitamin D).
Each of these hormones plays a unique and indispensable role in maintaining homeostasis and ensuring the proper functioning of other organ systems.
Understanding the hormone-producing capabilities of the kidneys is fundamental to appreciating their true importance in maintaining overall well-being. It is a crucial step in fully grasping the complexity of human physiology and the delicate balance required for optimal health.
Key Kidney Hormones and Their Vital Functions
We’ve established that the kidneys are far more than just waste disposal units. But what exactly are these "endocrine powerhouse" capabilities? The answer lies in the specific hormones the kidneys produce – each playing a vital, irreplaceable role in maintaining overall health.
This section will explore three of the primary hormones synthesized by the kidneys: erythropoietin (EPO), renin, and calcitriol (active vitamin D), detailing their individual functions and their significance in the symphony of bodily processes.
Erythropoietin (EPO): The Red Blood Cell Booster
Erythropoietin, or EPO, is a glycoprotein hormone with a critical mission: to stimulate red blood cell production in the bone marrow. This process, known as erythropoiesis, is the very foundation of our body’s ability to deliver oxygen to tissues and organs.
Without sufficient EPO, the bone marrow struggles to produce enough red blood cells, leading to anemia and its debilitating symptoms.
The Physiological Necessity of EPO
EPO’s role in preventing anemia extends far beyond simply alleviating fatigue. Adequate red blood cell production is essential for maintaining sufficient oxygen transport throughout the body.
Every cell, from the brain to the muscles, relies on a constant supply of oxygen to function properly. Insufficient oxygen delivery can lead to a cascade of problems, impacting everything from cognitive function and energy levels to physical performance and overall well-being.
EPO is not just helpful; it is a physiological necessity.
EPO and Chronic Kidney Disease (CKD)
Chronic kidney disease (CKD) often disrupts EPO production, leading to decreased EPO levels and subsequent anemia. As kidney function declines, the specialized cells responsible for synthesizing EPO become damaged, compromising their ability to produce this crucial hormone.
This connection between CKD and anemia is so strong that it is often one of the first signs of kidney dysfunction. The implications of decreased EPO levels in CKD patients are significant, contributing to fatigue, shortness of breath, and a reduced quality of life.
Treatment often involves synthetic EPO injections to stimulate red blood cell production.
Renin: The Blood Pressure Regulator
Renin is an enzyme released by the kidneys in response to decreased blood volume or blood pressure. It sets in motion a cascade of hormonal events known as the renin-angiotensin-aldosterone system (RAAS), a powerful mechanism for regulating blood pressure and fluid balance.
The Renin-Angiotensin-Aldosterone System (RAAS)
The RAAS pathway is a carefully orchestrated sequence of events. Renin initiates the process by converting angiotensinogen (a protein produced by the liver) into angiotensin I.
Angiotensin I is then converted to angiotensin II by angiotensin-converting enzyme (ACE), primarily found in the lungs. Angiotensin II is a potent vasoconstrictor, meaning it narrows blood vessels, thereby increasing blood pressure.
Angiotensin II also stimulates the release of aldosterone from the adrenal glands, which prompts the kidneys to retain sodium and water, further increasing blood volume and pressure.
Renin and Hypertension
While the RAAS is crucial for maintaining normal blood pressure, dysregulation of this system can lead to hypertension (high blood pressure). Overactivity of the RAAS, often due to underlying kidney disease or other factors, can cause excessive vasoconstriction and sodium retention, resulting in chronically elevated blood pressure.
Management strategies for hypertension often target the RAAS pathway. ACE inhibitors and angiotensin receptor blockers (ARBs) are commonly prescribed medications that interfere with the production or action of angiotensin II, helping to lower blood pressure.
Calcitriol: The Calcium Maestro (Active Vitamin D)
Calcitriol is the active form of vitamin D, a steroid hormone with a pivotal role in calcium regulation. While vitamin D is often associated with bone health, its active form, calcitriol, exerts far-reaching effects on calcium homeostasis throughout the body.
Calcitriol and Bone Health
Calcitriol is essential for maintaining healthy bones. It promotes the absorption of calcium from the intestines into the bloodstream, ensuring that the body has enough calcium to build and maintain strong bones.
It also works with parathyroid hormone (PTH) to regulate calcium levels in the blood. Without sufficient calcitriol, the body struggles to absorb calcium effectively, leading to weakened bones, increased risk of fractures, and other skeletal problems.
The Kidneys’ Role in Vitamin D Activation
The kidneys play a crucial role in converting inactive vitamin D, obtained from sunlight or dietary sources, into calcitriol. This conversion process involves a specific enzyme in the kidneys that adds a hydroxyl group to vitamin D, transforming it into its active hormonal form.
In individuals with kidney disease, this activation process is often impaired, leading to calcitriol deficiency and its associated consequences. Supplementation with calcitriol or specific vitamin D analogs is a common strategy to address this deficiency and maintain adequate calcium levels.
Key Kidney Hormones and Their Vital Functions
We’ve established that the kidneys are far more than just waste disposal units. But what exactly are these "endocrine powerhouse" capabilities? The answer lies in the specific hormones the kidneys produce – each playing a vital, irreplaceable role in maintaining overall health.
Interconnectedness: How Kidney Hormones Impact Whole-Body Health
The influence of kidney-derived hormones extends far beyond the confines of the urinary system. These potent chemical messengers exert a profound influence on seemingly disparate bodily functions, weaving a complex web of interconnectedness that underscores the kidney’s central role in maintaining systemic equilibrium.
Understanding these connections is paramount to appreciating the full scope of kidney health and recognizing the potential ramifications of hormonal imbalances.
Cardiovascular Harmony: Kidney Hormones and Blood Pressure
The kidneys are instrumental in maintaining healthy blood pressure through the intricate renin-angiotensin-aldosterone system (RAAS). Renin, released by the kidneys in response to low blood pressure or reduced sodium levels, initiates a cascade of events that ultimately lead to the production of angiotensin II.
Angiotensin II is a potent vasoconstrictor, narrowing blood vessels and increasing blood pressure. It also stimulates the release of aldosterone, a hormone that promotes sodium and water retention by the kidneys, further contributing to blood pressure elevation.
Dysregulation of the RAAS can lead to hypertension, a major risk factor for heart disease, stroke, and kidney damage. Conversely, proper kidney function and balanced hormone production are vital for maintaining optimal cardiovascular health.
Oxygen Delivery: EPO’s Systemic Impact
Erythropoietin (EPO), the kidney-produced hormone responsible for stimulating red blood cell production, plays a critical role in ensuring adequate oxygen delivery to all tissues and organs. Without sufficient EPO, the bone marrow struggles to produce enough red blood cells, leading to anemia.
Anemia, in turn, can cause fatigue, weakness, shortness of breath, and cognitive impairment, significantly impacting quality of life. The systemic impact of EPO extends to nearly every cell in the body, as oxygen is essential for cellular respiration and energy production.
Adequate EPO levels are therefore crucial for maintaining energy levels, cognitive function, and overall physical performance. The kidneys’ ability to produce EPO directly influences the vitality and well-being of the entire organism.
Calcium Regulation: Calcitriol’s Orchestration
Calcitriol, the active form of vitamin D synthesized by the kidneys, is a central player in calcium regulation. This hormone promotes calcium absorption in the intestine and helps maintain calcium balance in the bones.
Calcitriol deficiency can lead to weakened bones, increased risk of fractures, and other skeletal abnormalities. Furthermore, calcium dysregulation can have far-reaching consequences, affecting muscle function, nerve transmission, and blood clotting.
The kidneys’ role in converting inactive vitamin D to its active form is therefore essential for maintaining bone health and overall calcium homeostasis. The impact of calcitriol extends beyond the skeletal system, influencing a wide range of physiological processes.
The Symphony of Health: A Holistic View
The interconnectedness of kidney hormones highlights the importance of viewing health in a holistic manner. Dysfunction in one area can have cascading effects on other systems, underscoring the need for comprehensive assessment and management.
By understanding the far-reaching effects of kidney hormones, we can better appreciate the kidney’s central role in maintaining overall health and well-being. Recognizing these intricate connections is the first step towards proactive kidney care and preventing the potentially devastating consequences of hormonal imbalances.
Erythropoietin, renin, and calcitriol are crucial players in maintaining the body’s equilibrium. However, their delicate balance can be disrupted by a variety of factors, leading to significant health problems. Understanding the causes and consequences of these hormonal imbalances is paramount for effective management and prevention.
Kidney Hormone Imbalances: Causes, Consequences, and Symptoms
The intricate hormonal functions of the kidneys are susceptible to disruption, potentially triggering a cascade of adverse health effects. A multitude of factors can contribute to these imbalances, ranging from chronic diseases to genetic predispositions and lifestyle choices. These disruptions, in turn, can manifest as a spectrum of conditions, including anemia, hypertension, and debilitating bone disorders.
Factors Contributing to Kidney Hormone Imbalances
Several factors can disrupt the kidneys’ hormonal balance. Chronic kidney disease (CKD) is a primary culprit, as the progressive decline in kidney function directly impairs hormone production.
Diabetes, with its propensity to damage blood vessels, can also compromise the kidneys’ ability to synthesize and secrete hormones effectively.
Autoimmune diseases, such as lupus, can trigger inflammation and damage within the kidneys, interfering with their endocrine functions.
Certain medications, particularly NSAIDs and some blood pressure drugs, can also impact kidney function and hormone production. Genetic factors and inherited conditions can predispose individuals to kidney dysfunction and hormonal imbalances.
Erythropoietin (EPO) Deficiency
EPO deficiency is a common and significant consequence of kidney disease. EPO, produced by the kidneys, stimulates red blood cell production in the bone marrow.
Consequences of EPO Deficiency
When the kidneys are damaged, EPO production declines, leading to anemia. This anemia manifests as persistent fatigue, weakness, shortness of breath, and a generally diminished quality of life.
The body’s tissues and organs are deprived of adequate oxygen supply, impacting overall function and contributing to cardiovascular strain.
EPO Deficiency in Chronic Kidney Disease (CKD)
EPO deficiency is particularly prevalent in patients with CKD and renal failure. As kidney function deteriorates, the ability to produce EPO diminishes progressively, exacerbating anemia. Managing EPO deficiency is a critical aspect of CKD care, often involving synthetic EPO injections to stimulate red blood cell production.
Renin-Angiotensin System (RAS) Dysfunction
The renin-angiotensin system (RAS) is a complex hormonal pathway crucial for blood pressure regulation. Dysregulation of this system can lead to hypertension and cardiovascular complications.
How RAS Dysfunction Leads to Hypertension
When the RAS malfunctions, it can lead to excessive angiotensin II production, causing vasoconstriction and increased blood pressure.
Alternatively, the system may become insensitive to feedback mechanisms, leading to chronic hypertension.
Causes and Management of RAS Dysfunction
Several factors can contribute to RAS dysfunction, including kidney disease, genetic predisposition, and certain medications.
Management strategies typically involve lifestyle modifications such as dietary changes and exercise, along with medications like ACE inhibitors or ARBs to block the effects of angiotensin II.
Calcitriol Deficiency
Calcitriol, the active form of vitamin D, plays a crucial role in calcium regulation and bone health. The kidneys are responsible for converting inactive vitamin D into calcitriol.
Impaired Calcium Regulation and Bone Disorders
Calcitriol deficiency impairs calcium absorption from the gut, leading to low blood calcium levels. The body then compensates by drawing calcium from the bones, weakening them and increasing the risk of fractures and osteoporosis.
Other health issues related to Calcitriol deficiency can include increased risk for heart disease, some cancers, and cognitive decline.
Monitoring Vitamin D Levels in Kidney Disease
Patients with kidney disease are particularly vulnerable to calcitriol deficiency due to impaired kidney function.
Regular monitoring of vitamin D levels is essential, and supplementation with calcitriol or vitamin D may be necessary to maintain adequate calcium balance and bone health. Addressing calcitriol deficiency is vital for preventing bone disorders and improving overall well-being in patients with kidney disease.
Maintaining Kidney Hormone Balance: Lifestyle and Medical Strategies
The disruption of kidney hormone balance can have profound consequences, as detailed earlier. Fortunately, a proactive approach, encompassing both lifestyle modifications and targeted medical interventions, can significantly mitigate these risks and preserve kidney health.
Lifestyle Recommendations for Promoting Kidney Health
Adopting a kidney-friendly lifestyle is paramount in maintaining hormonal equilibrium and preventing dysfunction. These strategies are beneficial for both individuals with healthy kidneys and those with pre-existing kidney conditions.
Dietary Considerations
A carefully planned diet plays a crucial role in supporting kidney function. Limiting sodium intake is essential, as excessive sodium can elevate blood pressure, placing additional strain on the kidneys.
Processed foods are often high in sodium and should be consumed sparingly.
Maintaining adequate hydration is also vital. Water helps the kidneys flush out waste products and toxins, promoting optimal function. The recommended daily intake varies depending on individual factors such as activity level and climate, but aiming for at least eight glasses of water per day is a good starting point.
Protein intake should also be carefully monitored. While protein is essential for overall health, excessive consumption can burden the kidneys. Consulting a healthcare professional or registered dietitian is recommended to determine the appropriate protein intake based on individual needs and kidney function.
The Importance of Regular Exercise
Regular physical activity offers a multitude of benefits for kidney health. Exercise helps control blood pressure, manages blood sugar levels, and contributes to weight management, all of which are crucial for preventing kidney disease and its associated hormonal imbalances.
Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
Avoiding Nephrotoxic Substances
Exposure to nephrotoxic substances, which can damage the kidneys, should be minimized. This includes certain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), which should be used sparingly and under medical supervision.
Additionally, excessive alcohol consumption and smoking can negatively impact kidney function and should be avoided.
Medical Treatments for Addressing Kidney Hormone Imbalances
When lifestyle modifications are insufficient to restore hormonal balance, medical interventions may be necessary.
Erythropoietin-Stimulating Agents (ESAs)
For individuals with EPO deficiency-related anemia, erythropoietin-stimulating agents (ESAs) can be prescribed to stimulate red blood cell production. These medications help alleviate fatigue, improve energy levels, and enhance overall quality of life.
Careful monitoring of hemoglobin levels is essential during ESA therapy to avoid overcorrection and potential complications.
Management of the Renin-Angiotensin System
Dysfunction in the renin-angiotensin system (RAS) often leads to hypertension. Angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs) are commonly used to block the effects of the RAS, lowering blood pressure and protecting kidney function.
These medications require close monitoring by a healthcare professional to ensure optimal effectiveness and minimize side effects.
Vitamin D Supplementation and Calcitriol Therapy
Calcitriol deficiency can impair calcium regulation and bone health. Vitamin D supplementation, particularly in its active form (calcitriol), may be prescribed to correct this deficiency and promote calcium absorption.
Regular monitoring of calcium and parathyroid hormone levels is crucial during calcitriol therapy to prevent hypercalcemia.
Phosphate Binders
In advanced kidney disease, phosphate levels can become elevated, contributing to bone disorders and cardiovascular complications. Phosphate binders are medications that help reduce phosphate absorption in the gut, lowering serum phosphate levels and mitigating these risks.
Early Detection and Management of Chronic Kidney Disease (CKD)
Early detection and management of chronic kidney disease (CKD) are paramount in preventing hormonal dysfunction. CKD often progresses silently in its early stages, making regular screening, particularly for individuals with risk factors such as diabetes, hypertension, and family history of kidney disease, essential.
Regular monitoring of kidney function through blood and urine tests can help identify CKD in its early stages, allowing for timely interventions to slow its progression and prevent hormonal imbalances.
Managing underlying conditions such as diabetes and hypertension is also crucial, as these conditions are major contributors to CKD.
Kidney Hormones: Your Questions Answered
Here are some frequently asked questions to help you better understand the crucial role of kidney hormones in maintaining your body’s balance.
What exactly do kidney hormones do?
The hormones of kidney, such as erythropoietin (EPO) and calcitriol, are essential for regulating various bodily functions. EPO stimulates red blood cell production, preventing anemia. Calcitriol, the active form of vitamin D, helps regulate calcium absorption and bone health.
How do the kidneys produce these hormones?
Specialized cells within the kidneys are responsible for hormone production. In response to low oxygen levels, the kidneys release EPO. Similarly, the kidneys convert inactive vitamin D into calcitriol when signaled by parathyroid hormone (PTH). It’s a complex, highly regulated process.
What happens if the kidneys don’t produce enough hormones?
A deficiency in kidney hormone production can lead to several health problems. Low EPO results in anemia, causing fatigue and weakness. Reduced calcitriol can lead to bone problems like osteoporosis and an increased risk of fractures.
Can hormone imbalances from kidney issues be treated?
Yes, often these imbalances can be effectively managed. Synthetic EPO injections can boost red blood cell production for those with anemia. Calcitriol supplements can correct vitamin D deficiencies and improve calcium absorption, helping restore balance and improve health.
So, now you know a bit more about how your hormones of kidney are quietly working to keep everything humming along! Hopefully, this peek behind the scenes has been enlightening. Keep taking care of yourself!