Understanding the complex relationship between cellular hypoxia and irreversible tissue damage is critical in medicine. Ischemia and necrosis, two intertwined processes, are frequently observed following events like myocardial infarction, where the heart muscle is deprived of oxygen due to atherosclerosis. The resulting cellular death, or necrosis, is a key area of focus for researchers at institutions like the Mayo Clinic, who are diligently working to develop more effective strategies for prevention and treatment. Therefore, comprehending the multifaceted nature of ischemia and necrosis is essential for healthcare professionals and anyone interested in understanding the underlying causes of many common diseases.
Imagine a vital organ, starved of the very sustenance it needs to function. This is the reality of ischemia, a condition where blood supply is restricted, leading to a dangerous deprivation of oxygen and essential nutrients.
Untreated ischemia can trigger an even more devastating process: necrosis, or cell death. These two conditions, often intertwined, represent a significant threat to tissue health and overall well-being. Understanding their causes, consequences, and potential prevention strategies is crucial for safeguarding your health.
Understanding Ischemia and Necrosis
Ischemia and necrosis are fundamental concepts in understanding a wide range of diseases and injuries. They highlight the delicate balance required to maintain healthy tissue function and the potentially catastrophic consequences when that balance is disrupted.
Ischemia: A Blockage in the System
Ischemia occurs when the flow of blood to a tissue is reduced or completely blocked. This blockage prevents the delivery of oxygen and nutrients, which cells need to survive.
Think of it like a plant without water; it will slowly wilt and eventually die. Ischemia can result from various factors, ranging from narrowed arteries to blood clots, all impacting the vital delivery system within your body.
Necrosis: The Point of No Return
Necrosis is, in essence, cell death. It’s the result of irreversible damage caused by factors like prolonged ischemia, infection, or trauma.
Unlike apoptosis (programmed cell death), necrosis is a disorderly process that releases cellular contents into the surrounding tissue, triggering inflammation and potentially causing further damage. Different types of necrosis exist, each with its own characteristics and underlying causes.
Why This Matters to You
Ischemia and necrosis are not abstract medical concepts. They are at the root of many common and serious health problems, including heart attacks, strokes, and peripheral artery disease.
Recognizing the risks and understanding how to mitigate them can significantly impact your quality of life. This article aims to empower you with the knowledge you need to protect your tissues and maintain optimal health.
Our Objective
This article aims to provide a comprehensive overview of ischemia and necrosis. We will explore the underlying causes of these conditions, delve into their devastating consequences, and, most importantly, discuss strategies for prevention.
By understanding these processes, you can take proactive steps to reduce your risk and safeguard your well-being.
Imagine a vital organ, starved of the very sustenance it needs to function. This is the reality of ischemia, a condition where blood supply is restricted, leading to a dangerous deprivation of oxygen and essential nutrients.
Untreated ischemia can trigger an even more devastating process: necrosis, or cell death. These two conditions, often intertwined, represent a significant threat to tissue health and overall well-being. Understanding their causes, consequences, and potential prevention strategies is crucial for safeguarding your health.
Now, let’s delve deeper into the underlying mechanisms that trigger this cascade of events, from the initial blockage to the eventual cellular damage. We’ll explore the common culprits behind ischemia, how oxygen deprivation wreaks havoc on cells, which organs are most vulnerable, and even the paradoxical phenomenon of reperfusion injury.
The Mechanics of Ischemia: How Blood Flow Deprivation Leads to Tissue Damage
Ischemia, at its core, is a disruption of the body’s intricate circulatory system. It’s a situation where tissues are denied the life-sustaining oxygen and nutrients they desperately need.
Understanding the mechanics of ischemia means understanding the various ways blood flow can be compromised and the subsequent consequences for cellular health. Let’s examine these factors more closely.
Common Causes of Ischemia: A Cascade of Obstructions
Ischemia rarely arises spontaneously. It is usually the result of underlying conditions that directly impede blood flow. Here are the most frequent offenders:
-
Atherosclerosis and Plaque Formation: This is a gradual process where fatty deposits, cholesterol, and other substances accumulate within the artery walls. These plaques narrow the arteries, restricting blood flow and increasing the risk of clot formation. Atherosclerosis is a leading cause of ischemia in many organs, including the heart and brain.
-
Thrombosis and Blood Clot Formation: Thrombosis occurs when a blood clot forms inside a blood vessel, obstructing the flow of blood. These clots can form in arteries damaged by atherosclerosis or in veins due to sluggish blood flow.
-
Embolism and the Lodging of Clots in Vessels: An embolism happens when a blood clot, air bubble, or other foreign object travels through the bloodstream and becomes lodged in a smaller vessel, blocking blood flow to the area beyond the obstruction. Emboli often originate from the heart or large arteries.
-
External Compression of Blood Vessels: In some cases, blood vessels can be compressed from the outside, restricting blood flow. This can happen due to tumors, swelling, or even prolonged pressure on a limb.
Hypoxia: The Cellular Suffocation
Regardless of the cause, the ultimate consequence of ischemia is hypoxia, a state of reduced oxygen supply to the tissues. Oxygen is essential for cells to produce energy through a process called cellular respiration.
When oxygen levels plummet, cells are forced to switch to less efficient, anaerobic (without oxygen) metabolism. This leads to a buildup of lactic acid and other harmful byproducts, disrupting cellular function and eventually leading to cell death if the ischemia persists.
Vulnerable Organs: Where Ischemia Strikes Hardest
While any tissue can suffer from ischemia, some organs are particularly vulnerable due to their high metabolic demands and limited capacity for regeneration.
-
The Brain: The Specter of Stroke The brain is exquisitely sensitive to oxygen deprivation. Even a brief interruption of blood flow can lead to stroke, resulting in permanent brain damage, neurological deficits, and potentially death. Time is of the essence in stroke treatment, as prompt restoration of blood flow can minimize the extent of damage.
-
The Heart: The Crushing Grip of Myocardial Infarction The heart muscle, or myocardium, also relies on a constant supply of oxygen to function. When a coronary artery becomes blocked, the resulting ischemia can lead to myocardial infarction, commonly known as a heart attack. This causes damage or death of heart muscle tissue, impairing the heart’s ability to pump blood effectively.
Reperfusion Injury: A Paradoxical Twist
Ironically, restoring blood flow to an ischemic tissue can sometimes worsen the damage. This phenomenon, known as reperfusion injury, occurs because the sudden influx of oxygen and inflammatory cells can trigger a cascade of events that further harm the already vulnerable cells.
Oxidative stress, caused by the overproduction of free radicals, and inflammation play key roles in reperfusion injury. It’s a complex process that researchers are still working to fully understand.
Necrosis: The End Result of Untreated Ischemia
When ischemia persists, pushing cells beyond their limit to endure deprivation, the inevitable outcome is necrosis. Necrosis is not merely cell death, but a cascade of destructive events unfolding at the cellular level.
It’s a messy, uncontrolled process unlike apoptosis, which is programmed cell death, and it has significant consequences for the surrounding tissues and the body as a whole.
The Cellular Demise: A Step-by-Step Breakdown
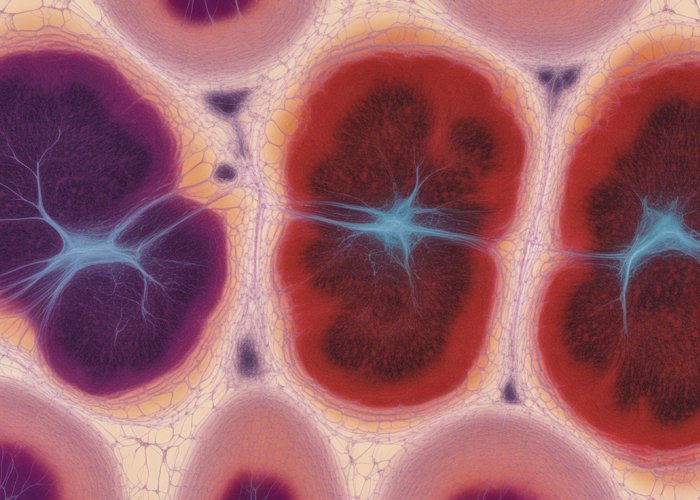
Necrosis is characterized by distinct morphological changes within the affected cells. Initially, cells begin to swell, a sign that their internal environment is becoming disrupted.
Cellular Swelling and Membrane Rupture
The cell membrane, normally a tightly regulated barrier, loses its integrity. This is because ion pumps that are reliant on ATP, that cannot be produced in ischemic conditions, cease to function, and cause osmotic imbalance. This leads to influx of water, and the swelling of organelles.
As the damage progresses, the cell membrane ruptures, spilling the cell’s contents into the surrounding tissue. This release of intracellular components triggers a significant inflammatory response.
Inflammation: A Double-Edged Sword
The inflammation caused by necrotic cell debris is a critical element of the process. While inflammation is initially intended to clear away the dead cells and initiate repair, the uncontrolled release of inflammatory mediators can further damage healthy tissue.
This is a delicate balance, where the body’s attempt to heal can inadvertently exacerbate the injury.
Types of Necrosis: A Spectrum of Destruction
Necrosis manifests in various forms, each characterized by unique features and associated with specific conditions.
Coagulative Necrosis
Coagulative necrosis is most commonly seen in solid organs such as the heart, kidneys, and liver. It is typically caused by infarction, or a blockage of blood supply, which leads to hypoxia.
The affected tissue retains its basic architecture for a period of time, but the cells are dead and their proteins denatured. The tissue often appears firm and pale.
Liquefactive Necrosis
Liquefactive necrosis is characterized by the digestion of dead cells, resulting in a liquid mass. This type of necrosis is common in the brain, where the tissue is rich in enzymes and has little structural support.
Bacterial infections can also lead to liquefactive necrosis, as immune cells release enzymes to combat the infection, also digesting the tissue. Pus formation is a hallmark of this type of necrosis.
Gangrene
Gangrene is a severe form of necrosis that results from a combination of ischemia and infection. It commonly affects the extremities, such as the toes, feet, and fingers.
Dry gangrene is characterized by dry, shrunken, and dark tissue, while wet gangrene involves bacterial infection and the accumulation of pus and fluid. Gangrene is a life-threatening condition that often requires amputation.
Consequences of Necrosis: Beyond the Cell
The consequences of necrosis extend far beyond the individual cells that die.
Organ Dysfunction
If a critical mass of cells within an organ undergoes necrosis, organ dysfunction can occur. The severity of the dysfunction depends on the extent of the necrosis and the importance of the affected tissue.
Systemic Inflammation and Sepsis
The release of intracellular contents and inflammatory mediators from necrotic tissue can trigger systemic inflammation, a body-wide response that can lead to sepsis.
Sepsis is a life-threatening condition characterized by organ dysfunction and a dysregulated immune response. It can lead to shock, organ failure, and death.
Death
In severe cases, extensive necrosis can lead to death. This is especially true when vital organs such as the heart, brain, or lungs are affected.
The understanding of necrosis is critical for developing effective strategies to prevent and treat ischemia, ultimately saving tissues and lives.
Specific Examples: Ischemia and Necrosis in Action
The abstract concepts of ischemia and necrosis take on stark reality when viewed through the lens of specific medical conditions. These processes, acting as silent adversaries within the body, can inflict devastating damage on various organ systems. Here, we explore some key examples, illustrating the far-reaching consequences of compromised blood supply and subsequent cell death.
Myocardial Infarction (Heart Attack)
Perhaps the most well-known example of ischemia and necrosis is myocardial infarction, commonly known as a heart attack. This occurs when a coronary artery, responsible for supplying blood to the heart muscle, becomes blocked.
The blockage is typically caused by a blood clot forming on top of a pre-existing plaque within the artery (atherosclerosis). This sudden obstruction cuts off oxygen and nutrient supply to a portion of the heart muscle.
The result is rapid ischemia, and if blood flow isn’t restored promptly, the affected heart cells undergo necrosis. The death of these cells impairs the heart’s ability to pump blood effectively.
The severity of a heart attack depends on the size and location of the blockage, as well as the speed at which medical intervention is received.
Stroke: Cerebral Ischemia and Necrosis
A stroke is essentially a "brain attack," and it shares a similar underlying mechanism with a heart attack: a disruption of blood flow. In the case of a stroke, the blockage occurs in an artery supplying the brain.
This can be caused by a blood clot (ischemic stroke) or a ruptured blood vessel (hemorrhagic stroke, which can also lead to ischemia due to compression). When brain tissue is deprived of oxygen and nutrients due to ischemia, neurons begin to die within minutes.
This rapid neuronal death leads to necrosis and subsequent neurological damage, which can manifest as a wide range of impairments, including paralysis, speech difficulties, and cognitive deficits. The location of the stroke in the brain determines the specific functions that are affected.
Peripheral Artery Disease (PAD)
Peripheral artery disease (PAD) is a condition in which the arteries that carry blood to the limbs, particularly the legs and feet, become narrowed or blocked. This is most commonly caused by atherosclerosis.
The reduced blood flow caused by PAD leads to ischemia in the affected limbs.
Initially, this may manifest as pain or cramping during exercise (intermittent claudication). However, as the disease progresses, the ischemia can become more severe, leading to chronic pain, non-healing ulcers, and, in the most severe cases, gangrene.
Gangrene is a form of necrosis complicated by bacterial infection. In advanced PAD, amputation of the affected limb may be necessary to prevent the spread of infection and save the patient’s life.
Bowel Ischemia: A Digestive Threat
Bowel ischemia refers to a condition in which the intestines do not receive enough blood flow. This can be caused by a variety of factors, including:
- Blood clots
- Narrowing of the arteries supplying the intestines
- Low blood pressure
The symptoms of bowel ischemia can vary depending on the severity and location of the reduced blood flow. Acute bowel ischemia, which occurs suddenly, can cause severe abdominal pain, bloody stools, and vomiting.
Chronic bowel ischemia, which develops gradually, may cause abdominal pain after eating, weight loss, and changes in bowel habits. If left untreated, bowel ischemia can lead to necrosis of the intestinal tissue. This can result in serious complications, such as peritonitis (inflammation of the abdominal lining) and sepsis.
Deep Vein Thrombosis (DVT) and Pulmonary Embolism
Deep vein thrombosis (DVT) occurs when a blood clot forms in a deep vein, usually in the legs. While DVT itself doesn’t directly cause necrosis in the vein, it can lead to complications that involve ischemia.
The primary concern with DVT is the risk of pulmonary embolism (PE). This happens when a portion or the entire blood clot breaks loose and travels through the bloodstream to the lungs, lodging in a pulmonary artery.
This blockage impedes blood flow to the lungs, causing ischemia and potential necrosis of lung tissue (pulmonary infarction). PE can be life-threatening, and prompt diagnosis and treatment are essential. Furthermore, chronic DVT can lead to post-thrombotic syndrome, causing chronic limb swelling, pain, and, in severe cases, skin ulcers due to impaired blood flow and venous hypertension.
Following the exploration of specific conditions where ischemia and necrosis wreak havoc, it’s crucial to understand how these threats are identified and combated. Early and accurate diagnosis, coupled with swift and effective treatment, are paramount in minimizing tissue damage and improving patient outcomes. The ability to recognize and intervene in these critical situations can literally be the difference between life and death, or between a full recovery and long-term disability.
Diagnosis and Treatment: Saving Tissues from the Brink
The diagnosis and treatment of ischemia and necrosis are crucial steps in mitigating tissue damage and improving patient outcomes. Early detection and timely intervention are paramount to saving tissues on the brink of irreversible damage. A multi-faceted approach involving advanced diagnostic tools and a range of treatment strategies is employed to restore blood flow and prevent further cellular demise.
Diagnostic Tools: Unveiling the Hidden Threat
Identifying ischemia and necrosis requires a sophisticated arsenal of diagnostic tools. These tools allow clinicians to visualize blood vessels, assess blood flow, and detect signs of tissue damage. The choice of diagnostic method depends on the suspected location and severity of the ischemia.
Angiography: Mapping the Vascular Landscape
Angiography remains a cornerstone in visualizing blood vessels and identifying blockages. This technique involves injecting a contrast dye into the bloodstream and then using X-rays to create images of the arteries.
Angiography can pinpoint the exact location and extent of a blockage, providing crucial information for treatment planning. Different forms of angiography exist, including traditional catheter angiography, CT angiography (CTA), and MR angiography (MRA), each with its own advantages and limitations. This helps determine the best method for blood flow restoration.
Doppler Ultrasound: Listening to the Flow
Doppler ultrasound is a non-invasive technique that assesses blood flow by measuring the change in frequency of sound waves reflected off red blood cells. It is particularly useful in evaluating blood flow in peripheral arteries and veins.
Doppler ultrasound can detect reduced or absent blood flow, indicating ischemia. It is also used to assess the severity of arterial stenosis (narrowing) and to monitor the effectiveness of treatments aimed at improving blood flow. Its non-invasive nature makes it a valuable tool for initial screening and follow-up assessments.
Other Diagnostic Modalities
Beyond angiography and Doppler ultrasound, other diagnostic tools may be employed depending on the clinical situation. These include:
-
Electrocardiogram (ECG): Used to detect electrical abnormalities in the heart, which can indicate myocardial ischemia.
-
Cardiac Enzyme Tests: Blood tests that measure levels of specific enzymes released by damaged heart muscle cells, confirming myocardial infarction.
-
Brain Imaging (CT or MRI): Used to visualize brain tissue and detect areas of infarction in patients suspected of stroke.
-
Biopsy: In certain cases, a tissue biopsy may be necessary to confirm the presence of necrosis and determine its cause.
Treatment Strategies: Restoring Blood Flow and Preserving Tissue
Once ischemia and necrosis are diagnosed, prompt treatment is essential to restore blood flow and prevent further tissue damage. Treatment strategies vary depending on the location and severity of the ischemia, as well as the overall health of the patient.
Thrombolysis: Dissolving the Deadly Clot
Thrombolysis involves the administration of drugs that dissolve blood clots, thereby restoring blood flow to the affected tissue. This is a critical treatment for acute ischemic events such as stroke and myocardial infarction.
The earlier thrombolysis is administered, the greater the chance of preventing irreversible tissue damage. These medications, often called "clot busters," must be used carefully due to the risk of bleeding.
Angioplasty: Opening Blocked Arteries
Angioplasty is a minimally invasive procedure used to widen narrowed arteries. It involves inserting a catheter with a balloon at its tip into the blocked artery. The balloon is then inflated, compressing the plaque against the artery wall and widening the vessel.
In many cases, a stent (a small, expandable mesh tube) is placed in the artery to help keep it open after the balloon is deflated. Angioplasty is commonly used to treat coronary artery disease, peripheral artery disease, and renal artery stenosis.
Bypass Surgery: Creating New Pathways
Bypass surgery involves creating new pathways for blood to flow around blocked arteries. This is typically done by grafting a healthy blood vessel from another part of the body (e.g., the leg or chest) onto the affected artery, bypassing the blockage.
Bypass surgery is often used to treat severe coronary artery disease and peripheral artery disease when angioplasty is not feasible or has failed. It can provide long-term relief from ischemia and improve quality of life.
Medications: Supporting Blood Flow and Preventing Clots
Medications play a crucial role in the treatment and prevention of ischemia and necrosis. These include:
-
Anticoagulants: Medications that prevent blood clots from forming, such as heparin and warfarin.
-
Antiplatelet Agents: Medications that prevent platelets from clumping together, reducing the risk of clot formation, such as aspirin and clopidogrel.
-
Vasodilators: Medications that widen blood vessels, improving blood flow, such as nitroglycerin and calcium channel blockers.
-
Statins: Medications that lower cholesterol levels, reducing the risk of atherosclerosis and plaque formation.
Adjunctive Therapies
In addition to the above strategies, other therapies may be used to support tissue recovery and prevent complications. These include:
-
Oxygen Therapy: Providing supplemental oxygen to improve tissue oxygenation.
-
Pain Management: Controlling pain associated with ischemia and necrosis.
-
Wound Care: Providing appropriate care for ischemic ulcers and gangrene.
-
Physical Therapy: Helping patients regain function and mobility after ischemic events.
The Importance of a Multidisciplinary Approach
The diagnosis and treatment of ischemia and necrosis require a multidisciplinary approach involving physicians, nurses, radiologists, and other healthcare professionals. Effective communication and collaboration among these team members are essential to ensure optimal patient care. Individualized treatment plans are developed based on the patient’s specific condition, risk factors, and preferences. The ultimate goal is to restore blood flow, prevent further tissue damage, and improve the patient’s overall quality of life.
Following the exploration of specific conditions where ischemia and necrosis wreak havoc, it’s crucial to understand how these threats are identified and combated. Early and accurate diagnosis, coupled with swift and effective treatment, are paramount in minimizing tissue damage and improving patient outcomes. The ability to recognize and intervene in these critical situations can literally be the difference between life and death, or between a full recovery and long-term disability.
Prevention: Reducing Your Risk of Ischemia and Necrosis
While medical interventions are crucial when ischemia and necrosis occur, the most impactful strategy is often prevention. By adopting a proactive approach to health and managing existing conditions, individuals can significantly reduce their risk of developing these dangerous conditions. Prevention focuses on modifying lifestyle choices and diligently controlling underlying health issues that contribute to vascular compromise.
Lifestyle Modifications: Building a Foundation for Vascular Health
Simple yet powerful lifestyle changes can profoundly impact vascular health and drastically reduce the likelihood of ischemic events. These modifications form the bedrock of preventive strategies.
Healthy Diet: Fueling Your Body, Protecting Your Arteries
A diet low in saturated and trans fats, cholesterol, and sodium is critical for maintaining healthy arteries. Focus on incorporating plenty of fruits, vegetables, whole grains, and lean protein sources.
Limiting processed foods is also essential, as they are often high in unhealthy fats, sodium, and added sugars that contribute to plaque buildup and inflammation. Embrace a Mediterranean-style diet, rich in olive oil, fish, nuts, and plant-based foods, which has been shown to have significant cardiovascular benefits.
Regular Exercise: Strengthening Your Heart, Enhancing Circulation
Physical activity is a cornerstone of vascular health. Regular exercise helps to improve circulation, lower blood pressure, and reduce cholesterol levels.
Aim for at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity exercise per week. Activities like brisk walking, swimming, cycling, and dancing are excellent choices. Even small amounts of physical activity are better than none, so find activities you enjoy and can incorporate into your daily routine.
Smoking Cessation: The Single Most Important Step
Smoking is a major risk factor for ischemia and necrosis. The chemicals in cigarette smoke damage blood vessels, increase blood clot formation, and reduce the amount of oxygen in the blood.
Quitting smoking is the single most impactful step you can take to protect your vascular health. If you smoke, seek help from your doctor or a smoking cessation program. There are many resources available to support you in quitting, including medications, counseling, and support groups.
Managing Underlying Conditions: Taking Control of Your Health
Effectively managing pre-existing conditions such as hypertension, diabetes, and high cholesterol is paramount in preventing ischemia and necrosis.
Controlling Blood Pressure: Preventing Hypertension’s Damaging Effects
High blood pressure (hypertension) puts excessive strain on blood vessel walls, leading to damage and increasing the risk of atherosclerosis and blood clot formation.
Regularly monitor your blood pressure and work with your doctor to keep it within a healthy range. This may involve lifestyle changes such as reducing sodium intake, exercising regularly, and maintaining a healthy weight. Medications are often necessary to effectively control blood pressure, so it’s crucial to follow your doctor’s recommendations.
Managing Diabetes: Protecting Against Blood Vessel Damage
Diabetes can damage blood vessels throughout the body, increasing the risk of both macrovascular (large vessel) and microvascular (small vessel) complications.
Careful blood sugar control is essential for preventing vascular damage. This involves a combination of diet, exercise, and medication, as prescribed by your doctor. Regular monitoring of blood sugar levels is crucial to ensure that blood sugar remains within a target range.
Lowering Cholesterol Levels: Preventing Plaque Buildup
High cholesterol levels, particularly high LDL ("bad") cholesterol, contribute to the formation of plaques in the arteries.
Lowering cholesterol levels through diet, exercise, and/or medication can significantly reduce the risk of atherosclerosis and subsequent ischemic events. A diet low in saturated and trans fats and high in fiber can help to lower cholesterol. Statins, a class of medications that lower cholesterol, are often prescribed for individuals at high risk of cardiovascular disease.
By prioritizing preventative measures, individuals can significantly reduce their susceptibility to ischemia and necrosis, paving the way for a healthier, more vibrant future.
Following the exploration of specific conditions where ischemia and necrosis wreak havoc, it’s crucial to understand how these threats are identified and combated. Early and accurate diagnosis, coupled with swift and effective treatment, are paramount in minimizing tissue damage and improving patient outcomes. The ability to recognize and intervene in these critical situations can literally be the difference between life and death, or between a full recovery and long-term disability.
Considering the significant impact of ischemia and necrosis on human health, research into new treatments and preventive strategies remains a crucial area of focus. The relentless pursuit of innovative solutions holds the promise of minimizing tissue damage and improving patient outcomes. Let’s examine some of the cutting-edge research and therapies poised to revolutionize the management of these conditions.
The Future of Ischemia and Necrosis Research
The landscape of ischemia and necrosis research is dynamic, with scientists and clinicians continually seeking new ways to prevent, diagnose, and treat these conditions. This section explores some of the most promising avenues of investigation, highlighting emerging therapies and ongoing research efforts that may shape the future of patient care.
Emerging Therapies: A New Hope for Tissue Preservation
The treatment of ischemia and necrosis is evolving beyond traditional methods, with emerging therapies offering the potential for more targeted and effective interventions. These innovative approaches aim to address the underlying causes of tissue damage and promote regeneration.
Cell-Based Therapies: Harnessing the Body’s Repair Mechanisms
Cell-based therapies represent a groundbreaking approach to treating ischemic damage. These therapies involve transplanting healthy cells, such as stem cells, into the affected tissue to promote healing and regeneration.
Stem cells have the remarkable ability to differentiate into various cell types, potentially replacing damaged cells and restoring tissue function. Research is underway to optimize stem cell delivery methods and enhance their regenerative capacity.
Initial studies have shown promise in treating conditions such as myocardial infarction and peripheral artery disease, with the goal of improving blood flow and reducing tissue necrosis. However, challenges remain in ensuring long-term cell survival and integration into the host tissue.
Targeted Drug Delivery: Precision Medicine for Ischemic Tissues
Traditional drug delivery methods often result in systemic exposure, which can lead to side effects and reduced efficacy. Targeted drug delivery systems aim to overcome these limitations by delivering therapeutic agents directly to the ischemic tissue.
Nanoparticles, liposomes, and other specialized carriers can be engineered to target specific cells or molecules within the affected area. This approach allows for higher drug concentrations at the site of injury while minimizing off-target effects.
For instance, researchers are developing nanoparticles that can deliver thrombolytic agents directly to blood clots, improving clot dissolution and reducing the risk of bleeding complications.
Novel Pharmacological Agents: Targeting the Ischemic Cascade
Beyond cell-based and delivery strategies, the discovery of new drugs that specifically target the molecular pathways involved in ischemia and necrosis is a burgeoning area of research. These agents aim to interrupt the damaging cascade of events that lead to cell death.
One promising approach involves developing inhibitors of specific enzymes or proteins that contribute to inflammation, oxidative stress, and apoptosis in ischemic tissues. These targeted therapies could potentially mitigate the severity of tissue damage and improve patient outcomes.
Focus Areas: Understanding the Mechanisms and Developing Strategies
Ongoing research efforts are focused on gaining a deeper understanding of the complex mechanisms underlying ischemia and necrosis. This knowledge is essential for developing more effective prevention and treatment strategies.
Elucidating the Molecular Mechanisms of Ischemic Injury
Researchers are actively investigating the molecular pathways involved in ischemic cell death, including the roles of hypoxia-inducible factors (HIFs), reactive oxygen species (ROS), and inflammatory cytokines.
By identifying key molecular targets, scientists can develop drugs that specifically modulate these pathways to protect tissues from ischemic damage. For example, research is exploring the potential of HIF stabilizers to enhance cellular adaptation to hypoxia and promote angiogenesis.
Developing Advanced Diagnostic Tools for Early Detection
Early detection is crucial for minimizing the extent of tissue damage in ischemia and necrosis. Researchers are working on developing advanced diagnostic tools that can detect subtle changes in tissue perfusion and cellular metabolism before irreversible damage occurs.
These tools include advanced imaging techniques, such as multispectral imaging and contrast-enhanced ultrasound, which can provide detailed information about tissue oxygenation and blood flow.
Additionally, researchers are exploring the use of biomarkers that can be detected in blood or other bodily fluids to identify individuals at risk of developing ischemia or necrosis.
Strategies for Promoting Tissue Regeneration and Repair
Beyond preventing further damage, research is also focused on developing strategies to promote tissue regeneration and repair after ischemic injury. This includes exploring the potential of growth factors, gene therapy, and biomaterials to stimulate tissue healing.
Growth factors are naturally occurring proteins that promote cell proliferation and differentiation. Researchers are investigating the use of growth factors to stimulate angiogenesis, promote tissue regeneration, and improve functional recovery after ischemic events.
The Importance of Personalized Medicine in Ischemia and Necrosis
As our understanding of ischemia and necrosis deepens, there is a growing recognition of the importance of personalized medicine. This approach takes into account individual patient characteristics, such as genetics, lifestyle, and medical history, to tailor treatment strategies to their specific needs.
By identifying individuals at high risk of developing ischemia or necrosis, healthcare professionals can implement preventive measures and monitor them closely for early signs of tissue damage. Additionally, personalized treatment plans can optimize the use of medications and therapies to maximize their effectiveness and minimize side effects.
Ischemia & Necrosis: Frequently Asked Questions
What’s the main difference between ischemia and necrosis?
Ischemia refers to a reduced blood supply to a tissue, depriving it of oxygen and nutrients. Necrosis is the death of cells and tissues that occurs as a consequence of prolonged or severe ischemia. Essentially, ischemia can lead to necrosis if left unaddressed.
Can necrosis be reversed?
Generally, no. Once cells have undergone necrosis, they are dead and cannot be revived. However, preventing further ischemia can limit the spread of necrosis and save surrounding tissues.
What are some common causes of ischemia?
Ischemia can result from various factors that block or narrow arteries. Common causes include blood clots, atherosclerosis (plaque buildup in arteries), and external compression of blood vessels. These conditions can lead to ischemia and eventually necrosis if severe enough.
How is necrosis treated?
Treatment for necrosis focuses on removing the dead tissue and preventing further damage. This may involve surgery to remove the necrotic tissue, antibiotics to combat infection, and addressing the underlying cause of the ischemia that led to the necrosis.
So, there you have it – a quick dive into the world of ischemia and necrosis! Hopefully, this gave you a clearer understanding of what’s going on inside the body when these events occur. Keep this knowledge in mind, and don’t hesitate to explore further if you’re curious.