Understanding the human body requires exploring fundamental tissues, and at the forefront of this exploration is the epithelial membrane. The study of histology, particularly at institutions like the Mayo Clinic, provides the framework for analyzing these membranes. Given its critical role in body functions, an epithelial membrane definition is crucial for grasping concepts such as permeability and understanding the barrier function it performs. By understanding how epithelial membranes function, researchers advance their knowledge of diseases such as cystic fibrosis, a condition where these membranes fail to work correctly.
Epithelial tissue: it’s a term you might not hear every day, but it represents a fundamental component of our bodies. From the surface of our skin to the lining of our internal organs, epithelial tissue acts as a crucial interface between our bodies and the external world.
This tissue forms continuous sheets, creating protective barriers and facilitating essential functions. Its presence is ubiquitous, a testament to its vital role in maintaining our health and well-being.
The Epithelial Membrane: A Boundary and Interface
Within the broader category of epithelial tissue lies the epithelial membrane. This specialized structure is more than just a simple covering; it’s a dynamic boundary.
It separates different compartments within the body and interacts with the external environment. Think of it as a highly selective gatekeeper.
It controls what enters and exits while protecting underlying tissues. Epithelial membranes line our digestive tract, allowing for nutrient absorption.
They also line our respiratory system, facilitating gas exchange. Furthermore, they cover our skin, preventing dehydration and infection.
These are just a few examples highlighting the diverse and critical roles these membranes play.
Why Understanding Epithelial Membranes Matters
Comprehending the structure and function of epithelial membranes is paramount in both physiology and pathology. In physiology, understanding these membranes helps us grasp how our bodies maintain homeostasis.
How they absorb nutrients, secrete hormones, and protect against harmful substances, are vital.
In pathology, disruptions in epithelial membrane function are often implicated in various diseases.
For example, certain cancers originate from epithelial cells, and understanding the mechanisms behind these transformations is crucial for developing effective treatments.
Similarly, inflammatory bowel disease involves damage to the epithelial lining of the intestines, leading to impaired absorption and barrier function.
By studying epithelial membranes, we can gain valuable insights into the mechanisms underlying these conditions and develop targeted therapies to restore normal function.
Furthermore, the study of epithelial membranes has implications for regenerative medicine and tissue engineering. Understanding how these membranes are structured and how they regenerate can help.
It can also lead to the development of new strategies for repairing damaged tissues and organs.
In essence, epithelial membranes are more than just cellular sheets; they are dynamic interfaces. They are critical for maintaining health and offer valuable insights into disease.
Disruptions in epithelial membrane function are often implicated in various diseases. For example, certain cancers originate from epithelial cells, and understanding how these cells lose their normal structure and behavior is crucial for developing effective treatments. Let’s now shift our focus to the intricate architecture and components that constitute epithelial membranes, revealing the secrets of their functionality.
Structure and Composition: A Deep Dive into Epithelial Membranes
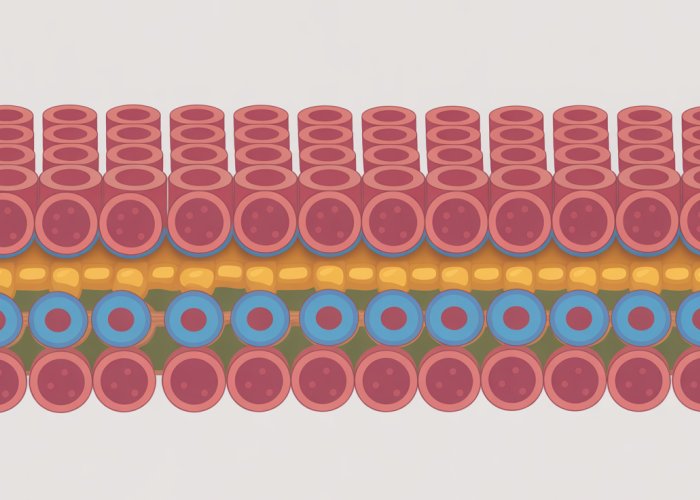
To truly appreciate the capabilities of epithelial membranes, we must delve into their structural foundation. This exploration encompasses cellular organization, the critical basement membrane, and the specialized cell junctions that bind everything together.
The Essence of Epithelial Tissue: Cellular Organization and Polarity
Epithelial tissue is defined by its distinct cellular organization. Cells are tightly packed together, forming a continuous sheet that acts as a barrier. This arrangement is crucial for its protective function.
Epithelial cells exhibit a property known as polarity, meaning they have distinct apical and basolateral surfaces.
The apical surface faces the external environment or the lumen of an organ. It is often specialized with structures like microvilli or cilia.
The basolateral surface interacts with adjacent cells and the underlying connective tissue. This polarity is fundamental to directional transport and other specialized functions.
The Basement Membrane: An Anchor and a Scaffold
Beneath the epithelial cells lies the basement membrane, a specialized extracellular matrix. It’s often overlooked but critically important.
This layer provides structural support and anchors the epithelial cells to the underlying connective tissue. Think of it as the foundation upon which the epithelial structure is built.
Composition and Function
The basement membrane is composed primarily of collagen, laminin, and other glycoproteins. These components assemble into a complex network.
This network provides both physical support and signaling cues to the epithelial cells. It influences cell differentiation, migration, and survival.
It also acts as a filter, controlling the passage of molecules between the epithelium and the underlying tissue.
Apical Specializations: Microvilli, Cilia, Keratin, and Goblet Cells
The apical surface of epithelial cells often features specialized structures that enhance their function. These specializations reflect the diverse roles these cells play in the body.
Microvilli are small, finger-like projections that increase the surface area for absorption. They are abundant in the small intestine, where nutrient uptake is essential.
Cilia are longer, hair-like structures that beat in a coordinated manner to move fluids or particles across the epithelial surface. They are found in the respiratory tract, where they help clear mucus and debris.
Keratin is a tough, fibrous protein that provides protection against abrasion and water loss. It is found in the epidermis, the outermost layer of the skin.
Goblet cells are specialized epithelial cells that secrete mucus. They are found in the respiratory and digestive tracts, where mucus lubricates and protects the lining.
Cell Junctions: The Glue That Holds It All Together
Epithelial cells are held together by specialized structures called cell junctions. These junctions are essential for maintaining the integrity and function of the epithelial barrier.
There are several types of cell junctions, each with a distinct structure and function. The main types are tight junctions, adherens junctions, and desmosomes.
Cell Junctions: Maintaining Integrity and Function
Cell junctions are not merely structural components; they are active participants in cell signaling and tissue organization. They influence cell shape, polarity, and differentiation.
The dynamic interplay between different types of junctions allows epithelial tissues to adapt to changing conditions and maintain their integrity.
Tight Junctions: Guardians of Permeability
Tight junctions form a seal between adjacent cells, preventing the passage of molecules between them. They are primarily found in epithelial cells.
They create a permeability barrier that controls what enters and exits the tissue. This barrier is critical for maintaining proper tissue function.
The tightness of these junctions can vary depending on the tissue type, reflecting the specific permeability requirements of each tissue.
Adherens Junctions and Desmosomes: Structural Support
Adherens junctions and desmosomes provide mechanical strength and stability to the epithelial tissue.
They anchor the cytoskeleton of adjacent cells together, distributing stress and preventing cell separation.
Adherens junctions are linked to actin filaments. Desmosomes are linked to intermediate filaments, like keratin.
These junctions are particularly important in tissues that are subjected to mechanical stress, such as the skin and the heart.
The basement membrane acts as a crucial interface, but above it, the epithelial cells themselves take center stage. These cells aren’t just a uniform mass; they exhibit remarkable diversity in both their arrangement and shape, leading to a sophisticated classification system that reflects their specialized functions. Understanding this classification is key to unlocking the secrets of epithelial membrane function.
Classifying Epithelial Membranes: A Comprehensive Overview of Types
Epithelial membranes are incredibly versatile, and to fully appreciate their diverse roles, we need a systematic way to categorize them. This classification primarily hinges on two key features: the number of cell layers present and the shape of the cells in the outermost layer.
This two-pronged approach allows us to precisely define each type of epithelium and understand its specific functional adaptations.
Classification Based on Cell Layer Arrangement
The arrangement of cells into layers is a fundamental characteristic used to classify epithelial tissues. We can broadly categorize them as either simple or stratified.
Simple Epithelium: A Single Layer of Efficiency
Simple epithelium is characterized by a single layer of cells, all of which are in direct contact with the basement membrane.
This arrangement is optimized for functions involving diffusion, absorption, secretion, and filtration. The thinness of the single layer facilitates the efficient transport of substances across the membrane.
Examples include the lining of blood vessels (endothelium) and the air sacs of the lungs (alveoli), where efficient gas exchange is paramount.
The main advantage is optimized diffusion, absorption, and filtration.
Stratified Epithelium: Strength in Numbers
In contrast to simple epithelium, stratified epithelium consists of two or more cell layers stacked upon each other.
The primary function of stratified epithelium is protection. The multiple layers provide a robust barrier against abrasion, friction, and other forms of physical stress.
The outer layers of cells are constantly being shed and replaced by cells from the underlying layers, ensuring the integrity of the tissue.
The significance of this structure is to provide physical protection to underlying tissues. Found in the epidermis of the skin, the lining of the mouth, and the esophagus.
Classification Based on Cell Shape
Beyond the number of layers, the shape of the cells in the outermost layer also plays a crucial role in determining the function of an epithelial membrane. The common shapes include squamous, cuboidal, and columnar.
Squamous Epithelium: Flattened for Diffusion
Squamous epithelium is composed of thin, flattened cells that resemble scales. The cells are wider than they are tall, with a flattened, disc-shaped nucleus.
This morphology is ideally suited for diffusion and filtration because it minimizes the distance substances need to travel across the membrane.
Primary functions include rapid diffusion, filtration, and some secretion.
Examples include the lining of blood vessels (endothelium) and the air sacs of the lungs (alveoli).
Cuboidal Epithelium: Specialized for Secretion and Absorption
Cuboidal epithelium consists of cells that are roughly cube-shaped, with a spherical, centrally located nucleus. These cells are approximately as tall as they are wide.
The morphology is specialized for secretion and absorption. These cells often have numerous organelles, such as mitochondria and ribosomes, which are essential for these processes.
Specialized roles include secretion and absorption in glands and kidney tubules.
Columnar Epithelium: Tall and Specialized for Absorption and Secretion
Columnar epithelium is characterized by cells that are taller than they are wide, resembling columns or pillars.
The nucleus is typically elongated and located near the base of the cell. This type of epithelium is often specialized for absorption and secretion.
Features include absorption, secretion of mucus and enzymes, and protection. The apical surface may be modified with microvilli to increase the surface area for absorption or with cilia to propel substances along the surface.
Examples include the lining of the stomach, intestines, and gallbladder.
Pseudostratified Columnar Epithelium: A Deceptive Arrangement
Pseudostratified columnar epithelium appears to be stratified (layered) at first glance, but in reality, it is a simple epithelium.
All cells are in contact with the basement membrane, but not all cells reach the apical surface. The nuclei are located at different levels, giving the illusion of multiple layers.
Unique characteristics include secretion and propulsion of mucus.
This type of epithelium is often found in the respiratory tract, where it is responsible for trapping and removing debris.
Transitional Epithelium: Adapting to Stretch
Transitional epithelium is a specialized type of stratified epithelium that is found in organs that need to stretch and distend, such as the urinary bladder.
The cells in this epithelium can change shape, transitioning from cuboidal or columnar when the organ is relaxed to flattened when the organ is stretched.
Location: Urinary bladder, ureters, and parts of the urethra.
The function is to allow distension of the urinary organs.
Glandular Epithelium: The Secretory Specialists
Glandular epithelium is specialized for secretion. These cells can be found individually or grouped together in glands.
Glands can be classified as either exocrine or endocrine, depending on how they release their secretions.
Exocrine glands secrete their products onto an epithelial surface via ducts (e.g., sweat glands, salivary glands).
Endocrine glands secrete their products (hormones) directly into the bloodstream (e.g., thyroid gland, pituitary gland).
Functions of Epithelial Membranes: A Multifaceted Role
Having categorized the diverse forms of epithelial membranes, we can now explore the impressive array of functions they perform within the body. These functions, tightly linked to their structural characteristics, are essential for maintaining homeostasis and enabling life processes. From forming protective barriers to facilitating complex transport mechanisms, epithelial membranes are truly multifunctional.
Protection: The Shielding Effect of Stratified Epithelia
Epithelial membranes are frequently found at the interface between the body and the external environment. As such, they often serve as a crucial protective barrier against physical abrasion, chemical damage, and pathogen invasion.
Stratified epithelia, with their multiple cell layers, are particularly well-suited for this role.
Squamous epithelium, in its stratified form, is a prime example. Found in the epidermis of the skin, it provides a robust shield against mechanical stress, desiccation, and harmful substances.
The outer layers of these cells are constantly being shed and replaced, effectively removing any accumulated damage and maintaining the integrity of the barrier.
The keratinized nature of the skin further enhances its protective capabilities, making it nearly impermeable to water and many other substances. This multi-layered structure is a testament to the importance of protection in specific regions of the body.
Absorption: Simple Epithelium and the Intestinal Tract
In contrast to the protective role of stratified epithelia, simple epithelia are often specialized for absorption. The single-cell layer facilitates the efficient transport of substances across the membrane.
The lining of the small intestine is a prime example, where simple columnar epithelium plays a critical role in nutrient absorption.
These cells are equipped with microvilli, tiny finger-like projections that vastly increase the surface area available for absorption.
This expanded surface area maximizes the contact between the epithelial cells and the digested nutrients, ensuring efficient uptake of essential molecules.
The close proximity of blood vessels to the epithelial layer further facilitates the rapid transport of absorbed nutrients into the bloodstream for distribution throughout the body. This illustrates the efficient design of the small intestine.
Secretion: Columnar, Cuboidal Epithelium and Goblet Cells
Many epithelial membranes are also involved in the secretion of various substances, including hormones, enzymes, mucus, and sweat.
The type of epithelium involved in secretion varies depending on the nature of the substance being secreted and the location of the gland.
Columnar epithelium, found in the lining of the stomach, secretes gastric juices that aid in digestion.
Cuboidal epithelium, found in glands such as the thyroid, secretes hormones that regulate various bodily functions.
Goblet cells, specialized secretory cells scattered throughout the respiratory and intestinal tracts, secrete mucus, a viscous fluid that lubricates and protects the epithelial surface.
This protective layer traps pathogens and debris, preventing them from reaching the underlying tissues. This process is crucial for maintaining a healthy internal environment.
Filtration and Diffusion: The Basement Membrane
While the epithelial cells themselves play a key role in many functions, the underlying basement membrane also contributes significantly, particularly in filtration and diffusion.
In the kidneys, for example, the basement membrane of the glomeruli acts as a selective filter, allowing small molecules like water, ions, and glucose to pass through while retaining larger molecules like proteins.
This filtration process is essential for the formation of urine and the removal of waste products from the blood.
In the lungs, the basement membrane facilitates the diffusion of oxygen and carbon dioxide between the air sacs (alveoli) and the blood vessels.
The thinness and permeability of the basement membrane are crucial for efficient gas exchange, ensuring that the body receives the oxygen it needs and eliminates waste carbon dioxide.
Simple epithelia, exemplified by the intestinal lining, showcase their absorptive capabilities, but what happens when these carefully orchestrated systems falter? The transition to understanding how epithelial membranes perform in healthy states leads us to exploring their clinical relevance in the context of disease. This connection is fundamental to understanding both the etiology of many common illnesses and how they manifest at a tissue level.
Clinical Relevance: Epithelial Membranes in Health and Disease
Epithelial membranes, far from being mere static barriers, are dynamic players in maintaining overall health. Their structure and function are intimately linked to the well-being of the tissues and organs they line. Understanding the clinical relevance of these membranes is therefore crucial for diagnosing, treating, and preventing a wide range of diseases.
The Interplay of Histology and Pathology
Histology, the study of tissues at a microscopic level, provides the foundational knowledge for understanding epithelial membranes. By examining the cellular architecture, organization, and characteristics of these membranes, we can establish a baseline for "normal" tissue structure.
Pathology, on the other hand, investigates the structural and functional changes in tissues and organs that result from disease. When epithelial membranes are affected by disease processes, their histological appearance can be significantly altered.
These alterations, observable under a microscope, can provide valuable clues for diagnosing the specific condition affecting the tissue. For example, changes in cell shape, size, or arrangement, the presence of inflammatory cells, or the disruption of the basement membrane can all indicate an underlying pathology.
Thus, histology provides the framework for understanding normal epithelial structure, while pathology utilizes this framework to identify and interpret abnormalities associated with disease.
Epithelial Dysfunction: A Gateway to Disease
The proper functioning of epithelial membranes is essential for maintaining homeostasis and preventing disease. When these membranes are compromised, a variety of pathological conditions can arise.
Epithelial dysfunction can manifest in several ways, including:
- Loss of barrier function: Allowing harmful substances or pathogens to penetrate underlying tissues.
- Impaired absorption: Leading to nutrient deficiencies.
- Abnormal secretion: Disrupting hormonal balance or digestive processes.
- Uncontrolled cell proliferation: Resulting in the formation of tumors.
Several diseases can directly be traced back to compromised epithelial membranes.
Cystic fibrosis, for instance, is characterized by a defect in a chloride channel present in epithelial cells lining the airways and other organs. This defect leads to the production of thick, sticky mucus that obstructs the airways and impairs lung function.
In celiac disease, the epithelial lining of the small intestine is damaged by an autoimmune response to gluten. This damage impairs nutrient absorption and leads to various gastrointestinal symptoms.
In contrast, certain cancers, like carcinomas, originate from epithelial cells that undergo uncontrolled proliferation. Mutations or gene expression abnormalities can trigger aberrant growth and invasion, leading to tumor formation and metastasis.
Diagnosis and Treatment: Leveraging Epithelial Insights
A thorough understanding of epithelial structure and function is critical for accurate diagnosis and effective treatment of various diseases.
Biopsies, for instance, often involve the examination of epithelial tissues to identify characteristic abnormalities that can confirm a diagnosis. The ability to differentiate between normal and abnormal tissue architecture is key to recognizing disease at an early stage.
Targeted therapies often focus on epithelial cells that have unique receptors or signaling pathways. By understanding these specific features, researchers can develop drugs that selectively target diseased epithelial cells while sparing healthy ones.
Regenerative medicine also seeks to harness the regenerative capabilities of epithelial tissues to repair damaged organs or tissues. Strategies like stem cell therapy and tissue engineering aim to stimulate epithelial cell proliferation and differentiation to restore tissue function.
Epithelial Membranes Across Organs: A Quick Tour
Epithelial membranes exhibit remarkable diversity, showcasing distinct functional roles across various organs.
Skin: The epidermis, a stratified squamous epithelium, provides a protective barrier against the external environment.
Lungs: Simple squamous epithelium in the alveoli facilitates gas exchange.
Intestines: Simple columnar epithelium with microvilli maximizes nutrient absorption.
Kidneys: Specialized epithelial cells in the nephrons perform filtration and reabsorption.
The specific structural and functional adaptations of epithelial membranes in each organ are crucial for their proper function.
The Supporting Role of Connective Tissue
While epithelial membranes form the primary interface with the external environment or internal body cavities, they do not operate in isolation. Connective tissue provides crucial structural support, nutrient supply, and immune defense for epithelial tissues.
The basement membrane, a specialized layer of extracellular matrix secreted by both epithelial and connective tissue cells, anchors the epithelium to the underlying connective tissue. This connection is essential for maintaining tissue integrity and facilitating cell-cell communication.
In addition, connective tissue contains blood vessels that supply oxygen and nutrients to epithelial cells, as well as immune cells that protect against infection. The interactions between epithelial and connective tissues are therefore crucial for maintaining tissue health and function.
Frequently Asked Questions About Epithelial Membranes
Here are some frequently asked questions about epithelial membranes and their functions.
What exactly is an epithelial membrane?
An epithelial membrane is a thin layer of tissue that covers the body’s external surfaces, lines internal cavities and organs, and forms glands. The epithelial membrane definition is essentially a boundary between different environments in the body.
How do epithelial membranes differ from other types of membranes?
Epithelial membranes are composed of tightly packed cells, unlike connective tissue membranes. They also have distinct apical (free) and basal (attached) surfaces, which differentiate them from other membrane types.
What are the different types of epithelial membranes and where are they found?
Epithelial membranes are broadly classified as cutaneous (skin), mucous (lining cavities open to the exterior, like the digestive tract), and serous (lining closed cavities, like the pleural cavity). Each type has specialized structures and functions depending on its location.
What are the primary functions of epithelial membranes?
Epithelial membranes serve multiple critical functions, including protection, absorption, secretion, and filtration. They act as a barrier protecting underlying tissues and regulate the passage of substances in and out of the body.
So, now you know a bit more about the epithelial membrane definition and what it does! I hope this helped clear things up, and you can now use this knowledge for your own studies or projects. Until next time!