Mastering EKG identification practice can seem daunting, but with focused effort, you can significantly improve your skills in just five days! Electrocardiography, a cornerstone of cardiology, relies heavily on accurate EKG interpretation. The American Heart Association emphasizes standardized training protocols for healthcare professionals. And remember, resources like the skillstat arrhythmia simulator are fantastic tools for hands-on learning; many find these simulations invaluable alongside the teachings of renowned experts such as Dr. Amal Mattu. The key is consistent, targeted ekg identification practice to confidently analyze heart rhythms and improve patient outcomes.
Imagine the scenario: a patient is rushed into the emergency room, clutching their chest, visibly distressed. In that critical moment, the ability to accurately and swiftly interpret their EKG can be the difference between life and death. EKG identification isn’t just a skill; it’s a responsibility – a cornerstone of effective patient care and positive outcomes in countless clinical settings.
This introduction sets the stage for a focused and efficient learning experience, designed to equip healthcare professionals with the knowledge and confidence they need to excel in EKG interpretation. We will briefly explore the fundamentals of EKGs and introduce a structured method for grasping cardiac rhythm interpretation.
The Critical Role of EKG Identification
An accurate EKG reading can rapidly pinpoint heart conditions that demand immediate attention.
From identifying subtle arrhythmias to detecting the telltale signs of a heart attack, your proficiency in EKG interpretation directly influences treatment decisions and patient outcomes.
In essence, mastering EKG identification empowers you to be a more effective and reliable healthcare provider.
What is an EKG?
An EKG, or electrocardiogram, is a non-invasive diagnostic tool that records the electrical activity of the heart over a period.
Electrodes are placed on the patient’s chest, arms, and legs to detect and amplify these electrical signals, producing a visual tracing that reflects the heart’s rhythm and function.
This tracing provides invaluable insights into various aspects of cardiac health, making the EKG an indispensable tool for diagnosing a wide range of heart conditions, including:
- Arrhythmias (irregular heartbeats)
- Myocardial infarction (heart attack)
- Ischemia (reduced blood flow to the heart)
- Conduction abnormalities
Introducing the 5-Day EKG Challenge
Given the crucial importance of EKG interpretation, it’s vital to have a systematic and effective learning approach. That’s why we’ve developed the "5-Day Challenge" – a focused, step-by-step program designed to help you rapidly acquire and refine your EKG identification skills.
This challenge breaks down the complexities of EKG interpretation into manageable daily modules, each building upon the previous one. Through a combination of:
- Concise explanations
- Practical exercises
- Real-world examples
You’ll gain the knowledge and confidence you need to accurately interpret EKGs in a variety of clinical settings.
Defining Cardiac Rhythm: The Heart’s Electrical Signature
At the heart of EKG interpretation lies the understanding of cardiac rhythm. Cardiac rhythm refers to the pattern and regularity of the heart’s electrical activity, as reflected on the EKG tracing.
A normal cardiac rhythm, known as sinus rhythm, indicates that the heart’s electrical impulses are originating from the sinoatrial (SA) node, the heart’s natural pacemaker.
However, various factors can disrupt this normal rhythm, leading to arrhythmias. Accurately identifying these arrhythmias is critical for guiding appropriate treatment decisions. The basic principles include:
- Rate: How fast or slow is the heart beating?
- Regularity: Are the heartbeats evenly spaced, or are they irregular?
- P Waves: Are P waves present, and do they precede each QRS complex?
- PR Interval: Is the PR interval within the normal range?
- QRS Complex: Is the QRS complex narrow or wide?
By systematically evaluating these characteristics, you can accurately determine the cardiac rhythm and identify any underlying abnormalities.
Day 1: Building a Solid Foundation in EKG Fundamentals
Having grasped the vital role EKG identification plays in healthcare and understood the basics of what an EKG is, we now turn to the critical first steps in mastering this essential skill. Day 1 focuses on equipping you with the foundational knowledge necessary to confidently interpret EKGs. We’ll dissect the components of a normal EKG tracing and introduce you to basic cardiac rhythms.
Understanding the EKG: A Window into the Heart’s Electrical Activity
An EKG, short for electrocardiogram (also abbreviated as ECG), is a non-invasive test that records the electrical activity of the heart.
Think of it as a visual representation of the heart’s electrical symphony.
By placing electrodes on the skin, the EKG machine detects and amplifies the tiny electrical signals generated by the heart as it beats.
This recording provides invaluable information about the heart’s rhythm, rate, and overall function, allowing healthcare professionals to identify abnormalities and diagnose a wide range of cardiac conditions.
Decoding the Waveform: Key Components Explained
The EKG tracing is composed of a series of waves, intervals, and segments, each representing a specific phase of the cardiac cycle. Understanding these components is crucial for accurate interpretation.
The P Wave: Atrial Depolarization
The P wave represents the electrical activity associated with the atria contracting, a process known as atrial depolarization.
It’s the first wave you’ll typically see in a normal EKG complex, a small upward deflection that indicates the atria are initiating the heartbeat.
The QRS Complex: Ventricular Depolarization
The QRS complex is a group of three waves (Q, R, and S) that represent the electrical activity associated with the ventricles contracting, called ventricular depolarization.
This is typically the largest and most prominent component of the EKG tracing.
The shape and duration of the QRS complex can provide valuable information about ventricular function and potential abnormalities.
The T Wave: Ventricular Repolarization
The T wave represents the electrical activity associated with the ventricles relaxing, a process known as ventricular repolarization.
It’s typically a positive (upward) deflection that follows the QRS complex.
Changes in the T wave’s shape or size can indicate various cardiac conditions, such as ischemia or electrolyte imbalances.
The PR Interval: Atrioventricular Conduction Time
The PR interval is the segment from the beginning of the P wave to the start of the QRS complex.
It represents the time it takes for the electrical impulse to travel from the atria through the AV node and into the ventricles.
A prolonged or shortened PR interval can indicate problems with AV node conduction.
The QT Interval: Ventricular Depolarization and Repolarization Time
The QT interval is measured from the beginning of the QRS complex to the end of the T wave.
It represents the total time it takes for the ventricles to depolarize and repolarize.
A prolonged QT interval can increase the risk of life-threatening arrhythmias.
The ST Segment: Period Between Depolarization and Repolarization
The ST segment is the section between the end of the QRS complex and the beginning of the T wave.
It represents the period when the ventricles are contracting but have not yet begun to relax.
Elevation or depression of the ST segment is a critical indicator of myocardial ischemia or infarction.
Heart Rate: Beats per Minute
Heart rate is simply the number of heartbeats per minute (BPM).
It can be easily calculated from the EKG tracing by measuring the distance between successive R waves.
A normal heart rate is typically between 60 and 100 BPM.
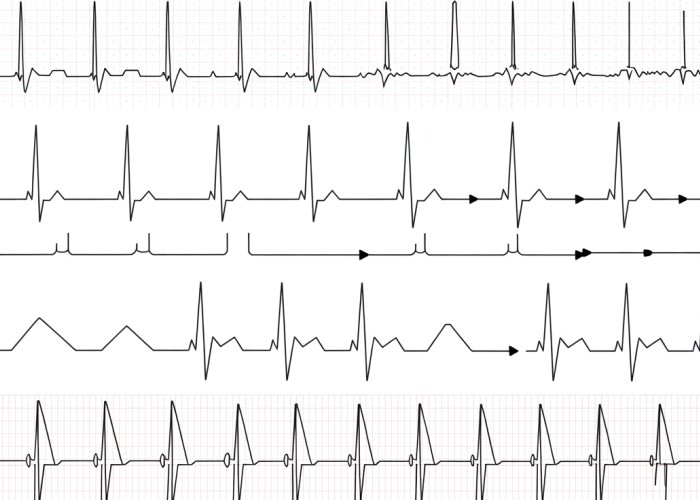
Fundamental Cardiac Rhythms: Recognizing the Basics
Understanding basic cardiac rhythms is essential for quickly assessing a patient’s heart function.
Normal Sinus Rhythm
Normal Sinus Rhythm (NSR) is the rhythm that originates from the sinoatrial (SA) node, which is the heart’s natural pacemaker.
It’s characterized by a regular heart rate between 60 and 100 BPM, a P wave preceding each QRS complex, and a consistent PR interval.
Sinus Bradycardia
Sinus Bradycardia is a sinus rhythm with a heart rate less than 60 BPM.
While it can be normal in athletes or during sleep, it can also indicate underlying cardiac issues.
Sinus Tachycardia
Sinus Tachycardia is a sinus rhythm with a heart rate greater than 100 BPM.
It can be caused by various factors, including exercise, stress, fever, or certain medications.
Practice Makes Perfect: EKG Practice Strips
Now that you’ve learned about the key waveform components and basic rhythms, it’s time to put your knowledge into practice! Using EKG practice strips, you can begin to identify waveforms and rhythms in a simulated environment.
This hands-on experience is crucial for developing your EKG interpretation skills and building confidence in your abilities.
Day 2: Advanced Waveform Analysis for Accurate Interpretation
Yesterday, we laid the groundwork for EKG interpretation by understanding the basic components of the waveform and identifying fundamental rhythms. Now, we move beyond the basics. Today, we refine our skills by diving into the nuances of each wave, interval, and segment. This involves examining their amplitude, duration, and morphology. Mastering these details is what separates a novice from a proficient EKG reader.
Decoding the Language of the Waveform: Amplitude, Duration, and Morphology
Waveform analysis is akin to learning the alphabet and grammar of the heart’s electrical language. Each characteristic – amplitude, duration, and morphology – provides crucial clues. These characteristics reveal insights into the heart’s health and potential pathologies.
Amplitude: Measuring the Signal Strength
Amplitude refers to the height or depth of a wave, measured in millivolts (mV). It reflects the strength of the electrical signal. Increased or decreased amplitude can signify various conditions, such as chamber enlargement or electrolyte imbalances.
Duration: Timing is Everything
Duration is the length of time a wave, interval, or segment lasts, measured in milliseconds (ms). Prolonged or shortened durations are often indicative of conduction delays or accelerated pathways within the heart.
Morphology: The Shape of the Wave
Morphology refers to the shape and form of the waveform. Changes in morphology, such as peaked T waves or notched P waves, can be telltale signs of specific cardiac abnormalities. Pay close attention to subtle variations in shape.
Distinguishing Normal from Abnormal: A Comparative Approach
The ability to differentiate between normal and abnormal waveforms is paramount for accurate interpretation. This skill comes with practice and a keen understanding of the expected parameters for each component.
Referencing established guidelines for normal ranges of amplitude and duration is essential. Deviations from these norms should raise suspicion and prompt further investigation.
Consider the clinical context. A slightly abnormal waveform in an otherwise healthy individual may be less concerning than the same finding in a patient with known heart disease.
The Significance of Intervals and Segments
While individual waves provide valuable information, intervals and segments offer a broader perspective on cardiac function. The PR Interval, QT Interval, and ST Segment are particularly significant in diagnosing various cardiac conditions.
PR Interval: Gauging Atrioventricular Conduction
The PR interval represents the time it takes for the electrical impulse to travel from the atria to the ventricles. A prolonged PR interval suggests a delay in conduction through the AV node, potentially indicating a heart block.
QT Interval: Ventricular Repolarization Time
The QT interval reflects the total time for ventricular depolarization and repolarization. A prolonged QT interval increases the risk of life-threatening arrhythmias, such as Torsades de Pointes. Factors like medications and electrolyte imbalances can affect the QT interval.
ST Segment: A Window into Myocardial Ischemia
The ST segment represents the period between ventricular depolarization and repolarization. ST elevation or depression is a hallmark sign of myocardial ischemia or infarction, demanding immediate attention. Prompt recognition can be life-saving.
Practice Makes Perfect: Analyzing Complex EKG Strips
Now, it’s time to put your knowledge into practice. Analyzing complex EKG strips is crucial for honing your skills and building confidence. Focus on identifying abnormalities in amplitude, duration, and morphology. Scrutinize the PR Interval, QT Interval, and ST Segment for any deviations from the norm.
Don’t be discouraged by initial challenges. EKG interpretation is a skill that improves with consistent effort and dedication. Approach each EKG strip as a puzzle waiting to be solved. Remember, every waveform tells a story – it’s your job to decipher it.
Decoding the Language of the Waveform: Amplitude, Duration, and Morphology
The ability to distinguish normal from abnormal EKG findings hinges on a comparative approach. Understanding the normal ranges and characteristics allows you to quickly identify deviations that may indicate underlying pathology. Let’s turn our attention to the irregularities – the arrhythmias – and learn to discern their unique signatures on the EKG.
Day 3: Mastering the Identification of Common Arrhythmias
Today, we shift our focus to the dynamic realm of cardiac arrhythmias. Arrhythmias, or irregular heartbeats, represent a significant departure from the heart’s normal electrical conduction. Spotting these patterns on an EKG is crucial for guiding appropriate and timely intervention. This section will serve as a detailed guide to understanding and identifying the most frequently encountered arrhythmias in clinical practice.
Understanding Arrhythmia Classifications
Arrhythmias are not a monolithic entity. To effectively diagnose and manage them, it’s essential to understand their origins and classifications. Arrhythmias are broadly categorized based on where they originate in the heart:
- Supraventricular Arrhythmias: These arrhythmias originate above the ventricles, typically in the atria or the AV node.
- Ventricular Arrhythmias: These arise from within the ventricles themselves. They are often more serious than supraventricular arrhythmias.
- Junctional Arrhythmias: Junctional arrhythmias originate in the AV junction. This is the area surrounding the AV node.
Understanding these classifications provides a framework for narrowing down the possible diagnoses when interpreting an EKG.
Common Arrhythmias: Characteristics and Clinical Implications
Let’s delve into some of the most common arrhythmias you’ll encounter in clinical practice, exploring their unique EKG characteristics and the implications for patient care:
Atrial Fibrillation (A-Fib)
- EKG Characteristics: Characterized by an absence of distinct P waves and an irregularly irregular R-R interval. Instead of P waves, you’ll see fibrillatory waves (f waves).
- Clinical Implications: Atrial fibrillation can lead to an increased risk of stroke due to blood clots forming in the atria. Rate control and anticoagulation are key management strategies.
Atrial Flutter
- EKG Characteristics: Presents with a characteristic "sawtooth" pattern of flutter waves (F waves) instead of P waves. The ventricular rate is typically regular or regularly irregular.
- Clinical Implications: Similar to atrial fibrillation, atrial flutter can increase the risk of stroke. Catheter ablation is often used to treat atrial flutter.
Ventricular Tachycardia (V-Tach)
- EKG Characteristics: Defined by a rapid, wide QRS complex tachycardia originating from the ventricles. P waves are usually absent or not associated with the QRS complexes.
- Clinical Implications: Ventricular tachycardia can be life-threatening. It can quickly degenerate into ventricular fibrillation, which can lead to sudden cardiac death. Prompt treatment, including cardioversion or antiarrhythmic medications, is essential.
Ventricular Fibrillation (V-Fib)
- EKG Characteristics: A chaotic, irregular rhythm with no discernible P waves, QRS complexes, or T waves. It represents a complete loss of coordinated ventricular activity.
- Clinical Implications: Ventricular fibrillation is a lethal arrhythmia. It requires immediate defibrillation to restore a perfusing rhythm.
Case Studies: Putting Theory into Practice
The best way to solidify your understanding of arrhythmia identification is through real-world examples. Reviewing case studies, complete with EKG tracings, can help you connect the theoretical knowledge with actual clinical scenarios. Work through examples of each arrhythmia. Pay close attention to the subtle nuances that differentiate one rhythm from another. Online resources, textbooks, and EKG interpretation courses often provide valuable case studies for practice.
Leveraging EKG Simulators for Skill Development
EKG simulators are a fantastic tool for honing your rhythm interpretation skills in a safe and controlled environment. These simulators allow you to practice identifying various arrhythmias without the pressure of a live patient scenario. Many simulators offer adjustable settings. These settings allow you to customize the complexity of the rhythms. This will help you progress from basic identification to more advanced interpretations. Regular use of EKG simulators can significantly boost your confidence and accuracy in real-world situations.
By mastering the identification of common arrhythmias, you’ll be well-equipped to recognize potentially life-threatening conditions. This will allow you to contribute meaningfully to patient care. Remember, consistent practice and a commitment to continuous learning are key to becoming a proficient EKG interpreter.
Day 4: Recognizing Critical Cardiac Events on the EKG
Having explored the landscape of arrhythmias and their diverse presentations on the EKG, we now turn our attention to identifying acute cardiac events, where timely recognition and intervention can be life-saving.
This section is dedicated to mastering the EKG signs of myocardial infarction (MI), commonly known as a heart attack, and understanding how to differentiate between ischemia and infarction patterns.
Identifying Myocardial Infarction (MI) on the EKG
The EKG serves as a critical tool in the early diagnosis of MI. Recognizing the subtle but crucial changes on the EKG tracing is paramount for initiating appropriate treatment strategies. The hallmark signs of MI include:
-
ST-segment elevation: This is arguably the most specific EKG finding for acute ST-elevation myocardial infarction (STEMI).
The ST segment, which represents the period between ventricular depolarization and repolarization, will appear elevated above the baseline.
-
ST-segment depression: While often associated with non-STEMI or ischemia, ST depression can also be seen in reciprocal leads during STEMI.
-
T-wave inversion: Inverted T waves can indicate ischemia or injury to the heart muscle.
They may appear early in the course of an MI or persist even after other EKG changes have resolved.
The presence and location of these EKG changes, in conjunction with the patient’s clinical presentation, are vital for accurate diagnosis and risk stratification.
Recognizing Ischemia and Infarction Patterns
It is essential to distinguish between ischemia (reduced blood flow) and infarction (tissue death) on the EKG.
-
Ischemia typically manifests as T-wave inversions or ST-segment depression.
-
Infarction is characterized by ST-segment elevation (in the acute phase) and the possible development of Q waves, which represent irreversible myocardial damage.
The evolution of these EKG patterns over time provides valuable information about the extent and duration of myocardial injury.
Understanding the specific lead locations and the corresponding areas of the heart they represent is crucial for localizing the infarction and predicting potential complications.
The Urgency of Timely Intervention
In acute cardiac events, time is muscle.
The sooner an MI is diagnosed and treated, the greater the chance of preserving heart muscle and improving patient outcomes.
Rapid recognition of EKG changes suggestive of MI should trigger immediate action, including notification of the appropriate medical team and initiation of guideline-directed therapy.
Don’t underestimate your role in the chain of survival; your ability to recognize these patterns can significantly impact a patient’s life.
Resources for Nurses and Medical Students
To further enhance your knowledge and skills in EKG interpretation, numerous resources are available. Consider exploring:
-
American Heart Association (AHA): The AHA offers comprehensive courses and materials on EKG interpretation, including advanced cardiac life support (ACLS) training.
-
Online EKG simulators: These interactive tools provide realistic practice scenarios for identifying various cardiac rhythms and abnormalities.
-
Textbooks and journal articles: Consult reputable cardiology textbooks and peer-reviewed articles for in-depth information on EKG interpretation and management of cardiac conditions.
-
Continuing education courses: Attend workshops and conferences to stay updated on the latest advancements in EKG interpretation and cardiac care.
Rhythm Interpretation in Acute Cardiac Events
Accurate rhythm interpretation is paramount in the context of acute cardiac events. Arrhythmias such as ventricular tachycardia or fibrillation can occur during MI, requiring immediate intervention.
Proficiency in identifying these life-threatening rhythms on the EKG is essential for nurses and medical students to provide optimal care to patients experiencing acute cardiac emergencies.
Remember, consistent practice and ongoing learning are key to mastering EKG interpretation and confidently recognizing critical cardiac events.
Day 5: Synthesis, Continuous Learning, and Long-Term Skill Development
Having dedicated the past few days to dissecting EKG waveforms, identifying arrhythmias, and recognizing critical cardiac events, it’s time to consolidate your newfound knowledge and chart a course for continued growth. This final day is about weaving together all the threads of information, honing your practical skills, and establishing a framework for lifelong learning in the dynamic field of EKG interpretation.
Solidifying Your Foundation: A Comprehensive Review
Let’s begin by revisiting the core principles that underpin accurate EKG interpretation. This isn’t merely a rote recap, but rather an opportunity to actively reinforce your understanding. Reflect on the fundamental waveform components – the P wave, QRS complex, and T wave – and their intricate relationship to the heart’s electrical activity.
Consider how alterations in amplitude, duration, or morphology can signal underlying cardiac abnormalities. Review the characteristics of normal sinus rhythm and the key distinguishing features of common arrhythmias like atrial fibrillation, ventricular tachycardia, and heart blocks.
Think back to the EKG signs of myocardial infarction, including ST elevation, ST depression, and T-wave inversions. This comprehensive review serves as the bedrock upon which your future expertise will be built.
Sharpening Your Skills: Advanced EKG Practice
Theory alone is insufficient to master EKG interpretation. Practical application is paramount. Therefore, this section presents advanced EKG practice strips designed to challenge your diagnostic acumen and push you beyond your comfort zone.
These challenging cases present complex scenarios that require you to synthesize your knowledge of waveforms, intervals, and rhythms to arrive at an accurate diagnosis. Don’t be discouraged if you encounter difficulties; instead, view them as opportunities for growth and refinement.
Carefully analyze each EKG strip, systematically evaluating the P waves, QRS complexes, T waves, PR intervals, and QT intervals. Consider the clinical context and any available patient history to inform your interpretation. The goal is not simply to arrive at the correct answer, but to develop a rigorous and methodical approach to EKG analysis.
The Path to Mastery: Continuous Learning and Staying Updated
The field of cardiology is constantly evolving, with new research, guidelines, and technologies emerging at a rapid pace. To remain proficient in EKG interpretation, it’s essential to embrace a mindset of continuous learning and actively seek out opportunities to stay updated on the latest advances.
Key Resources for Continuing Education
The American Heart Association (AHA) is a leading authority on cardiovascular health and offers a wealth of resources for healthcare professionals, including courses, guidelines, and publications related to EKG interpretation.
Numerous online platforms, such as Medscape, UpToDate, and ECG Wave-Maven, provide access to articles, tutorials, and interactive quizzes to enhance your knowledge and skills.
Consider subscribing to relevant journals and attending conferences to stay abreast of the latest research and best practices in the field.
Cultivating Expertise: Tips for Long-Term Skill Development
Beyond formal education and training, there are several practical steps you can take to foster long-term skill development in EKG interpretation.
- Regular Practice: Dedicate time each week to review EKG strips and analyze clinical cases.
- Seek Mentorship: Find an experienced cardiologist or EKG technician who can provide guidance and feedback.
- Teach Others: Explaining EKG concepts to colleagues or students can reinforce your own understanding.
- Embrace Challenges: Don’t shy away from complex or ambiguous EKG tracings; instead, use them as opportunities to learn and grow.
- Utilize Technology: Leverage EKG simulators and online resources to practice in a realistic and interactive environment.
Final Encouragement: Embrace the Journey
Mastering EKG interpretation is a journey, not a destination. There will be times when you feel overwhelmed or discouraged, but don’t give up. Remember why you embarked on this path – to provide the best possible care for your patients.
Your dedication to mastering EKG interpretation can have a profound impact on the lives of those you serve. Embrace the challenges, celebrate your successes, and never stop learning. The world needs skilled EKG experts like you.
Your journey to EKG mastery begins now. Good luck!
EKG Identification Practice: Frequently Asked Questions
Here are some common questions about improving your EKG identification skills, especially if you’re aiming to master them in a short timeframe.
What exactly does "EKG identification practice" involve?
EKG identification practice is the process of repeatedly analyzing electrocardiograms (EKGs or ECGs) to recognize patterns and identify cardiac abnormalities. This includes recognizing normal rhythms, arrhythmias, and signs of ischemia or infarction. Consistent ekg identification practice is key to becoming proficient.
What makes the 5-day timeframe realistic?
The 5-day timeframe assumes focused, deliberate practice. This involves dedicating specific time each day to studying EKG examples, using practice quizzes, and reviewing challenging concepts. Consistent effort over 5 days can lead to noticeable improvements in ekg identification practice.
What resources are recommended for effective EKG identification practice?
Effective resources include EKG textbooks, online EKG simulators, and practice quizzes. Utilizing a variety of resources provides a well-rounded approach to ekg identification practice. Look for resources that offer feedback on your interpretations.
How can I track my progress during my EKG identification practice?
Track your progress by noting your accuracy on practice quizzes and identifying areas where you struggle. Regular self-assessment is crucial to identify your weaknesses and tailor your ekg identification practice accordingly.
Alright, you’ve got the knowledge! Now go out there and confidently tackle those EKGs. Remember, consistent practice is key to acing that ekg identification practice. Good luck, and happy interpreting!