Hypercalcemia, a condition characterized by elevated calcium levels in the blood, significantly impacts cardiac function. Cardiac electrophysiology, a specialized field, studies the mechanisms of these impacts, particularly as reflected in ECG interpretation. Understanding ecg changes hypercalcaemia requires careful assessment, where even subtle variations in the electrocardiogram can provide crucial diagnostic clues. Institutions like the American Heart Association emphasize standardized protocols for ECG recording and interpretation to ensure accurate diagnosis. Ultimately, a deep knowledge of calcium homeostasis is essential to understanding the effects of hypercalcemia on the heart and properly identifying these subtle changes.
Hypercalcemia, characterized by elevated levels of calcium in the blood, represents a significant clinical concern due to its potential to disrupt various physiological processes. While the condition can stem from a multitude of underlying causes, its impact on cardiac function is particularly noteworthy.
Studies suggest that hypercalcemia affects a notable portion of the population, with some research indicating a prevalence of up to 1-2% in certain clinical settings. This underscores the importance of understanding its potential effects, especially those detectable through electrocardiography (ECG).
The Urgency of ECG Recognition
Prompt recognition of ECG changes associated with hypercalcemia is not merely academic; it is crucial for timely medical intervention. The heart, a finely tuned bioelectrical machine, relies on a delicate balance of electrolytes, including calcium, to function correctly.
Elevated serum calcium can throw this balance into disarray, leading to a cascade of cardiac complications. Recognizing these changes early allows for prompt treatment, which can prevent severe outcomes and improve patient prognosis.
Calcium’s Direct Impact on Cardiac Function
The connection between elevated serum calcium levels and cardiac dysfunction is direct and profound. Calcium ions play a pivotal role in the heart’s electrical and mechanical activity, influencing both the conduction of electrical impulses and the force of myocardial contraction.
When calcium levels rise excessively, the heart’s normal rhythm and function can be significantly impaired. This can manifest as a variety of ECG abnormalities, ranging from subtle alterations in the QT interval to more pronounced changes in T-wave morphology. These changes, if left unaddressed, can progress to life-threatening arrhythmias or even cardiac arrest.
The heart’s ability to pump blood relies on an intricate choreography of electrical signals and muscular contractions, a process where calcium ions play a starring role. To truly grasp the significance of hypercalcemia’s impact, it’s essential to understand the fundamental influence calcium exerts on the heart’s normal function. Let’s delve into how these ions orchestrate the electrical symphony within the heart and why their balance is critical.
Calcium’s Role: The Electrical Symphony of the Heart Explained
The heart, at its core, is a sophisticated pump driven by precisely timed electrical impulses and coordinated muscle contractions. Calcium ions are indispensable in both of these processes. Their presence, concentration, and movement across cell membranes dictate the rhythm and strength of each heartbeat.
Calcium’s Influence on Cardiac Conduction
Cardiac conduction is the process by which electrical impulses are generated and spread throughout the heart, triggering sequential contractions of the atria and ventricles.
Calcium ions are essential for the automaticity of the sinoatrial (SA) node, the heart’s natural pacemaker. In these cells, a slow influx of calcium ions during diastole (the resting phase) gradually depolarizes the cell membrane, eventually reaching a threshold that triggers an action potential.
This action potential then propagates through specialized conduction pathways, ultimately leading to ventricular contraction. Calcium also plays a crucial role in the upstroke of the action potential in the SA and AV nodal cells.
Role of Calcium Channels
Voltage-gated calcium channels, particularly L-type calcium channels, are critical in mediating the influx of calcium during the action potential.
The opening of these channels allows a rapid influx of calcium ions, which further depolarizes the cell and contributes to the overall amplitude and duration of the action potential.
Calcium’s Impact on Cardiac Muscle Contraction and Relaxation
Beyond electrical conduction, calcium is the primary trigger for cardiac muscle contraction itself. This process, known as excitation-contraction coupling, involves a complex interplay of proteins and ions.
-
Calcium Influx: When an action potential reaches a cardiac muscle cell (cardiomyocyte), it triggers the opening of L-type calcium channels in the cell membrane (sarcolemma). This allows extracellular calcium to enter the cell.
-
Calcium-Induced Calcium Release (CICR): The influx of calcium from the sarcolemma triggers the release of even greater amounts of calcium from the sarcoplasmic reticulum (SR), an intracellular calcium store. This process is known as calcium-induced calcium release (CICR).
-
Binding to Troponin: The surge in intracellular calcium concentration causes calcium ions to bind to troponin C, a protein located on the thin filaments (actin) of the sarcomere.
-
Cross-Bridge Cycling: This binding causes a conformational change in the troponin-tropomyosin complex, exposing the myosin-binding sites on actin. Myosin heads can then bind to actin, forming cross-bridges.
-
Muscle Contraction: The myosin heads pivot, pulling the actin filaments towards the center of the sarcomere, resulting in muscle contraction. ATP is then used to detach the myosin heads, allowing the cycle to repeat.
Relaxation: For the heart muscle to relax, calcium must be removed from the cytoplasm. This is primarily achieved through:
- The sarcoplasmic reticulum calcium ATPase (SERCA) pump, which actively transports calcium back into the SR.
- The sodium-calcium exchanger (NCX), which exchanges calcium for sodium across the cell membrane.
- Plasma membrane calcium ATPase (PMCA).
The Critical Importance of Electrolyte Balance
Maintaining a delicate balance of electrolytes, particularly calcium, is crucial for optimal heart function. Even slight deviations from the normal range can have profound effects on cardiac electrical and mechanical activity.
Hypocalcemia (low calcium) can prolong the QT interval and weaken cardiac contractions, while hypercalcemia (high calcium), as discussed earlier, can shorten the QT interval and increase the risk of arrhythmias.
The heart’s sensitivity to calcium levels underscores the importance of understanding and managing electrolyte imbalances in patients with cardiac conditions. Maintaining proper electrolyte balance is not simply a matter of "normal" lab values; it’s about optimizing the cellular environment in which the heart functions.
When electrolyte balance is disturbed, the heart’s electrical and mechanical efficiency suffers, potentially leading to life-threatening complications. Understanding the specific role of calcium in the heart’s symphony of activity is key to appreciating the significance of ECG changes associated with hypercalcemia.
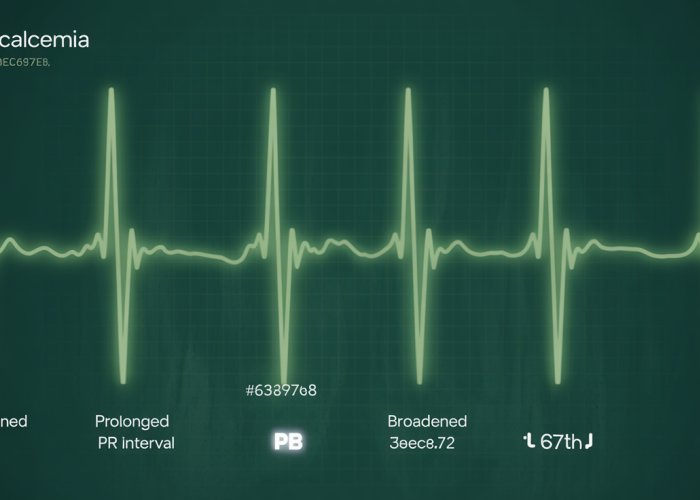
Decoding the Hypercalcemic ECG: Key Changes to Watch For
Having established the vital role calcium plays in the heart’s electrical activity, we now turn our attention to the electrocardiogram (ECG) and how hypercalcemia manifests on this crucial diagnostic tool. Understanding these ECG changes is paramount for the timely recognition and management of hypercalcemia, ultimately preventing potentially life-threatening cardiac complications.
The ECG is an indispensable tool for evaluating heart function. It provides a visual representation of the heart’s electrical activity, allowing clinicians to identify abnormalities in rhythm, conduction, and repolarization. In the context of hypercalcemia, the ECG serves as a window into the heart’s response to elevated calcium levels, revealing telltale signs of cardiac dysfunction.
The ECG as a Window into Heart Function
The ECG records the electrical impulses as they travel through the heart. Deviations from the norm, such as changes in the shape or duration of waveforms, can indicate underlying pathology. The ECG can detect a wide range of cardiac conditions, from arrhythmias to ischemia, making it an invaluable tool in both emergency and routine clinical settings.
Hypercalcemia’s Fingerprint: Recognizing the Signs
Hypercalcemia leaves a distinct imprint on the ECG, primarily through two key changes: QT interval shortening and T-wave abnormalities. Recognizing these changes is critical, as they can be subtle, particularly in mild cases of hypercalcemia. A systematic approach to ECG interpretation, with a heightened awareness of the potential for hypercalcemic changes, is essential.
QT Interval Shortening: A Hallmark of Hypercalcemia
One of the most characteristic ECG findings in hypercalcemia is a shortened QT interval. The QT interval represents the time from the start of ventricular depolarization (Q wave) to the end of ventricular repolarization (T wave).
How Hypercalcemia Shortens the QT Interval
Hypercalcemia accelerates ventricular repolarization, effectively reducing the duration of the QT interval. This shortening occurs because elevated extracellular calcium levels increase the driving force for calcium influx into cardiac cells during repolarization. This accelerated repolarization leads to a briefer action potential duration, and consequently, a shorter QT interval on the ECG.
ECG Examples of QT Interval Shortening
A normal QT interval varies depending on heart rate and gender, but generally falls within the range of 0.36 to 0.44 seconds. In hypercalcemia, the QT interval may be significantly shorter than the lower limit of normal, sometimes dropping below 0.30 seconds.
Visual examples are invaluable for recognizing this subtle change. Look for instances where the T wave appears to rise almost immediately after the S wave, with minimal ST segment elevation. Comparing the patient’s current ECG with previous recordings, if available, can also help identify a new or progressive shortening of the QT interval.
The Physiology Behind the Abnormality
The QT interval shortening is a direct result of calcium’s influence on the myocardial action potential. Elevated extracellular calcium levels enhance the activity of calcium-activated potassium channels.
This increased potassium efflux further contributes to the rapid repolarization and shortening of the action potential duration. Understanding this underlying mechanism helps to solidify the connection between hypercalcemia and the observed ECG changes.
T Wave Abnormalities: Another Clue
In addition to QT interval shortening, hypercalcemia can also induce changes in the morphology of the T wave. One of the most commonly observed T-wave abnormalities is the development of peaked T waves.
Peaked T Waves in Hypercalcemia
Peaked T waves are characterized by their increased amplitude and narrow base. They differ from the broad, rounded T waves typically seen in healthy individuals. These peaked T waves are particularly prominent in the precordial leads (V1-V6) on the ECG.
Visual Examples of T Wave Changes
ECG examples demonstrating peaked T waves associated with hypercalcemia are essential for pattern recognition. Look for T waves that are taller and narrower than normal, with a sharp, pointed appearance. The presence of peaked T waves, in conjunction with QT interval shortening, should raise strong suspicion for hypercalcemia.
Careful observation of the T wave morphology, combined with an assessment of the QT interval, is crucial for accurately interpreting the ECG in the context of suspected hypercalcemia. These subtle changes, when recognized promptly, can lead to earlier diagnosis and improved patient outcomes.
Dangerous Rhythms: Hypercalcemia’s Impact on Heart Rhythm
While shortened QT intervals and altered T-wave morphology provide clues to hypercalcemia’s presence on the ECG, the most concerning manifestations often involve disturbances in the heart’s fundamental rhythm. Elevated calcium levels can significantly disrupt the delicate balance of electrical activity, increasing the risk of both arrhythmias and bradycardia. Understanding these risks is crucial for clinicians, as these rhythm disturbances can rapidly progress to life-threatening scenarios.
Arrhythmia Risk in Hypercalcemia
Hypercalcemia significantly elevates the risk of developing various types of arrhythmias. These irregular heartbeats stem from the way excess calcium interacts with the heart’s electrical pathways.
The increased calcium concentration affects the refractory period of cardiac cells. This alteration can lead to early afterdepolarizations, which in turn trigger abnormal heart rhythms.
Atrial fibrillation, atrial flutter, and ventricular arrhythmias are among the most concerning possibilities. These arrhythmias can compromise cardiac output and lead to hemodynamic instability.
In individuals with pre-existing heart conditions, the risk of developing hypercalcemia-induced arrhythmias is particularly pronounced. Thus highlighting the importance of careful monitoring in these vulnerable populations.
Bradycardia and Hypercalcemia: A Slowing Heart
Beyond accelerating the heart rate with arrhythmias, hypercalcemia can paradoxically cause bradycardia, a dangerously slow heart rate. This effect is complex and multifaceted.
Elevated calcium levels can directly affect the sinoatrial (SA) node. The SA node is the heart’s natural pacemaker. Calcium’s influence can suppress its activity, leading to a slower heart rate.
Hypercalcemia can also enhance vagal tone, further contributing to bradycardia. This is because increased calcium can sensitize the heart to the effects of the vagus nerve, which slows heart rate.
Severe bradycardia can result in decreased blood flow to the brain and other vital organs. This can manifest as dizziness, syncope (fainting), or even more severe neurological complications.
The Threat of Cardiac Arrest and the Importance of Monitoring
In severe, untreated cases, hypercalcemia can precipitate cardiac arrest, the abrupt cessation of heart function. This catastrophic outcome underscores the urgency of early detection and management.
The mechanisms leading to cardiac arrest are complex. They often involve a combination of severe arrhythmias and profound bradycardia. These result in ineffective cardiac output.
Continuous cardiac monitoring is paramount in patients with known or suspected hypercalcemia. This is because the ECG allows for the real-time detection of rhythm disturbances.
Prompt identification of arrhythmias or bradycardia enables timely intervention, preventing progression to cardiac arrest and significantly improving patient outcomes. In critical cases, advanced cardiac life support (ACLS) protocols must be readily available.
Clinical Implications: Recognizing and Responding to Hypercalcemic ECG Changes
Having explored the ECG manifestations of hypercalcemia, including shortened QT intervals, T-wave abnormalities, and the potential for dangerous arrhythmias, it is crucial to shift our focus towards the practical application of this knowledge in clinical settings. The ability to promptly recognize these ECG changes during cardiac monitoring is not merely an academic exercise; it’s a cornerstone of effective hypercalcemia management and ultimately, improved patient outcomes.
The Critical Role of ECG Recognition in Hypercalcemia Detection
Early detection of hypercalcemia via ECG monitoring is paramount. The ECG serves as a readily available and non-invasive tool, providing real-time insights into the heart’s electrical activity.
A keen awareness of the ECG changes associated with hypercalcemia enables clinicians to suspect the condition early, prompting further investigation and timely intervention.
This is especially critical in patients at high risk, such as those with malignancy, primary hyperparathyroidism, or those receiving certain medications known to elevate calcium levels. Continuous cardiac monitoring, coupled with a vigilant approach to ECG interpretation, can significantly reduce the risk of severe cardiac complications.
Managing Hypercalcemia: A Multifaceted Approach
Once hypercalcemia is suspected or confirmed, a comprehensive management strategy is essential to mitigate the risk of cardiac complications and address the underlying cause. The specific approach will depend on the severity of the hypercalcemia and the patient’s overall clinical status.
Here are key steps in managing hypercalcemia:
- Immediate Discontinuation of Offending Medications: Review the patient’s medication list and discontinue any drugs known to contribute to hypercalcemia, such as thiazide diuretics or calcium-containing supplements.
- Volume Expansion with Intravenous Fluids: Administering intravenous fluids, typically normal saline, helps to dilute the serum calcium concentration and promote calcium excretion via the kidneys.
- Loop Diuretics: Following volume expansion, loop diuretics, such as furosemide, can be used to further enhance calcium excretion.
- Bisphosphonates: These medications inhibit osteoclast activity, thereby reducing bone resorption and lowering serum calcium levels. They are particularly useful in managing hypercalcemia associated with malignancy.
- Calcitonin: Calcitonin directly inhibits bone resorption and promotes calcium excretion. Its effects are rapid but transient, making it a useful adjunct to other therapies.
- Dialysis: In severe cases of hypercalcemia, especially when accompanied by renal insufficiency, dialysis may be necessary to rapidly lower serum calcium levels.
Treatment Strategies and Considerations
The selection of appropriate treatment strategies necessitates careful consideration of the patient’s clinical picture and underlying etiology. For instance, hypercalcemia secondary to primary hyperparathyroidism might eventually require surgical intervention (parathyroidectomy). Hypercalcemia in the setting of malignancy may necessitate treatment directed at the underlying cancer.
It is important to note that aggressive treatment of hypercalcemia is not without risks. Rapid correction of serum calcium levels can lead to hypocalcemia and other electrolyte imbalances. Therefore, close monitoring of serum calcium, electrolytes, and renal function is essential throughout the management process.
Ultimately, effective management of hypercalcemia requires a multidisciplinary approach, involving close collaboration between physicians, nurses, and other healthcare professionals. By promptly recognizing ECG changes and implementing appropriate treatment strategies, clinicians can significantly reduce the risk of severe cardiac complications and improve outcomes for patients with hypercalcemia.
Hypercalcemia ECG Changes: Frequently Asked Questions
[Hypercalcemia can lead to noticeable changes on an electrocardiogram (ECG). Here’s a breakdown of some common questions and answers to help you understand these changes.]
What specific ECG changes are commonly seen in hypercalcemia?
The most common ecg changes hypercalcaemia includes a shortened QT interval. You might also see prolonged PR intervals and widened QRS complexes in severe cases. T wave abnormalities can also occur.
Why does hypercalcemia affect the QT interval?
Hypercalcemia speeds up ventricular repolarization. This results in the QT interval getting shorter on the ECG. This is a primary indicator of ecg changes hypercalcaemia.
At what calcium level do ECG changes typically start to appear?
ECG changes hypercalcaemia are more likely to be visible when serum calcium levels rise significantly above the normal range. Often, changes begin to appear when calcium exceeds 12 mg/dL, but individual sensitivity can vary.
What is the clinical significance of recognizing hypercalcemia-related ECG changes?
Recognizing ecg changes hypercalcaemia is crucial for prompt diagnosis and treatment. Severe hypercalcemia can lead to life-threatening arrhythmias. Early identification can prevent serious complications.
So, there you have it! Hopefully, you now have a better grasp of what to look for when it comes to ecg changes hypercalcaemia. Now, go forth and be a calcium-detecting ECG whiz!