Differential diagnosis in bone lesions radiology often hinges on precise radiographic interpretation. Magnetic Resonance Imaging (MRI), a crucial modality, offers superior soft tissue contrast, aiding in characterizing lesion composition. The American College of Radiology (ACR) provides established guidelines for imaging protocols and reporting standards, ensuring consistency in clinical practice. Histopathological correlation, often guided by the Lodwick-Madewell grading system, is paramount for definitive diagnosis, especially in cases of suspected malignancy. This visual guide will explore these key aspects, providing a comprehensive overview of bone lesions radiology for practitioners and students alike.
Crafting the Ideal Article Layout: "Bone Lesions Radiology: Your Complete Visual Guide!"
This document outlines an effective article layout designed to provide a comprehensive understanding of bone lesions radiology. The structure prioritizes clarity, visual learning, and easy navigation, ensuring the reader can quickly locate specific information related to “bone lesions radiology.”
I. Introduction: Setting the Stage
The introduction should immediately define "bone lesions" and explain the role of radiology in their diagnosis. It should briefly touch upon the different imaging modalities involved and their relative strengths and weaknesses.
- What are bone lesions? Provide a simple, layman’s definition and categorize them broadly (e.g., benign vs. malignant).
- Why Radiology? Explain why radiological imaging is crucial in detecting, characterizing, and staging bone lesions.
- Scope of the Guide: Briefly outline what the article will cover, setting realistic expectations for the reader.
II. Imaging Modalities in Bone Lesion Evaluation
This section will detail the various imaging techniques used in "bone lesions radiology," including their principles, advantages, and limitations.
A. Plain Radiography (X-rays)
- Principles: Explain the basic physics of X-ray imaging.
- Advantages: Cost-effective, readily available, good for initial screening.
- Limitations: Low sensitivity for subtle lesions, poor soft tissue contrast.
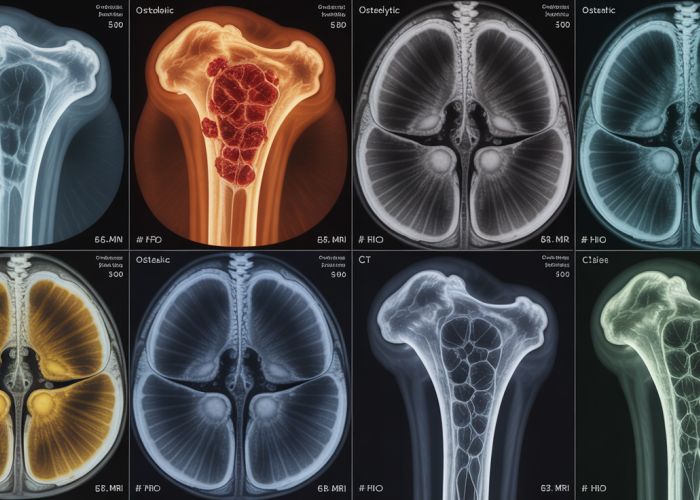
- Visual Examples: Include representative X-ray images demonstrating various bone lesions (e.g., lytic lesions, sclerotic lesions).
B. Computed Tomography (CT)
- Principles: Explain how CT creates cross-sectional images using X-rays.
- Advantages: Superior bony detail compared to plain radiography, allows for 3D reconstruction.
- Limitations: Higher radiation dose, can be limited in assessing marrow involvement.
- Visual Examples: CT images showcasing bone matrix mineralization, cortical destruction, and periosteal reaction.
C. Magnetic Resonance Imaging (MRI)
- Principles: Explain how MRI utilizes magnetic fields and radio waves to generate images.
- Advantages: Excellent soft tissue contrast, superior for assessing marrow involvement, no ionizing radiation.
- Limitations: More expensive, longer acquisition times, contraindications for patients with certain metallic implants.
- Visual Examples: MRI images demonstrating bone marrow edema, soft tissue extension of a lesion, and neurovascular involvement.
D. Bone Scintigraphy (Bone Scan)
- Principles: Explain how bone scans use radiopharmaceuticals to detect areas of increased bone turnover.
- Advantages: Highly sensitive for detecting early bone lesions, useful for screening for metastases.
- Limitations: Low specificity, cannot differentiate between benign and malignant lesions.
- Visual Examples: Bone scan images showing areas of increased radiotracer uptake.
E. Other Modalities (Briefly Mentioned)
- PET/CT: Positron Emission Tomography combined with CT.
- Ultrasound: Limited role, but can be useful for guiding biopsies.
III. Describing Bone Lesions: A Radiological Approach
This section focuses on the specific characteristics radiologists use to describe bone lesions on imaging. This is vital for narrowing the differential diagnosis.
A. Location
- Epiphyseal: Located in the epiphysis (end) of the bone.
- Metaphyseal: Located in the metaphysis (between the epiphysis and diaphysis).
- Diaphyseal: Located in the diaphysis (shaft) of the bone.
- Intra-articular: Extending into the joint space.
B. Size and Shape
- Measurements: How to accurately measure lesion dimensions on different imaging modalities.
- Description of Shape: Round, oval, lobulated, irregular.
C. Margins
- Well-defined: Sharp, clear borders, suggesting a slower-growing lesion.
- Ill-defined: Indistinct borders, suggestive of a more aggressive process.
D. Bone Matrix
- Lytic: Bone destruction, appearing dark on X-rays and CT.
- Sclerotic: Bone formation, appearing bright on X-rays and CT.
- Mixed Lytic and Sclerotic: A combination of bone destruction and formation.
- Ground Glass: A hazy, homogeneous density.
E. Periosteal Reaction
- Solid: Continuous layer of new bone formation.
- Lamellated (Onion Skin): Multiple layers of new bone formation.
- Spiculated (Sunburst): Radial pattern of new bone formation.
- Codman Triangle: A triangular area of elevated periosteum.
F. Soft Tissue Extension
- Presence or Absence: Whether the lesion extends beyond the confines of the bone.
- Extent of Involvement: Describing the size and location of any soft tissue mass.
IV. Specific Bone Lesions: Visual Examples and Radiological Features
This is the core of the "Visual Guide" and should be the most extensive section. This section should be organized by likely etiology or by imaging appearance for ease of access.
A. Benign Bone Lesions
- Osteochondroma: Include typical X-ray and MRI features.
- Radiological Features: Cartilage cap, continuity with the underlying bone.
- Visual Examples: Annotated images highlighting key features.
- Enchondroma: Include typical X-ray and MRI features.
- Radiological Features: Lytic lesion with chondroid matrix.
- Visual Examples: Annotated images highlighting key features.
- Fibrous Dysplasia: Include typical X-ray and CT features.
- Radiological Features: Ground-glass appearance, shepherd’s crook deformity.
- Visual Examples: Annotated images highlighting key features.
- Bone Cyst (Simple and Aneurysmal): Include typical X-ray and MRI features.
- Radiological Features: Fluid-filled lesion, thin rim of sclerosis (simple), multiple fluid-fluid levels (aneurysmal).
- Visual Examples: Annotated images highlighting key features.
- Giant Cell Tumor: Include typical X-ray and MRI features.
- Radiological Features: Epiphyseal location, lytic lesion with well-defined but non-sclerotic margins.
- Visual Examples: Annotated images highlighting key features.
B. Malignant Bone Lesions
- Osteosarcoma: Include typical X-ray, CT, and MRI features.
- Radiological Features: Aggressive lytic and sclerotic lesion, Codman triangle, soft tissue mass.
- Visual Examples: Annotated images highlighting key features.
- Ewing Sarcoma: Include typical X-ray and MRI features.
- Radiological Features: Diaphyseal location, onion-skin periosteal reaction, moth-eaten appearance.
- Visual Examples: Annotated images highlighting key features.
- Chondrosarcoma: Include typical X-ray, CT, and MRI features.
- Radiological Features: Chondroid matrix mineralization (rings and arcs), cortical destruction.
- Visual Examples: Annotated images highlighting key features.
- Metastases: Include typical bone scan, X-ray, CT, and MRI features.
- Radiological Features: Multiple lytic or sclerotic lesions, often in the axial skeleton.
- Visual Examples: Annotated images highlighting key features.
- Multiple Myeloma: Include typical X-ray and MRI features.
- Radiological Features: Multiple "punched-out" lytic lesions, diffuse osteopenia.
- Visual Examples: Annotated images highlighting key features.
Note: Each lesion should include:
- A brief description of the lesion.
- Typical age and location.
- Radiological features on different imaging modalities.
- Key differential diagnoses.
V. Reporting Bone Lesions: A Structured Approach
This section provides guidance on how to structure a radiology report for bone lesions.
A. Key Elements of a Report
- Patient Demographics: Age, sex, relevant clinical history.
- Imaging Modality: Which imaging studies were performed.
- Location and Size: Precise description of the lesion’s location and dimensions.
- Morphology: Detailed description of the lesion’s appearance (margins, matrix, periosteal reaction, etc.).
- Differential Diagnosis: A list of potential diagnoses based on the radiological findings.
- Recommendations: Suggestions for further evaluation (e.g., biopsy, follow-up imaging).
B. Example Report Template
Provide a sample radiology report template that can be adapted for different bone lesions.
Patient: [Patient Name]
Study: [Imaging Modality]
Findings:
There is a [Size] lesion located in the [Location]. The lesion is [Description of Margins - e.g., well-defined/ill-defined] and demonstrates [Description of Bone Matrix - e.g., lytic/sclerotic] characteristics. The periosteal reaction is [Description - e.g., solid/lamellated/absent]. There is/is not evidence of soft tissue extension.
Differential Diagnosis:
Based on the above findings, the differential diagnosis includes: [List of Differential Diagnoses]
Recommendations:
[Recommendations for further evaluation]
Bone Lesions Radiology: Frequently Asked Questions
Here are some common questions about bone lesions radiology and how to interpret radiological images. We hope this helps clarify some common points.
What exactly is a bone lesion?
A bone lesion refers to any abnormality or area of damaged tissue within a bone. These can be benign (non-cancerous) or malignant (cancerous). Bone lesions radiology plays a critical role in determining the nature and extent of these lesions.
How is radiology used to identify bone lesions?
Various imaging techniques, including X-rays, CT scans, MRI, and bone scans, are used in bone lesions radiology. These tools help visualize the bone structure and identify abnormalities like growths, fractures, or areas of bone destruction.
What are the typical signs of a malignant bone lesion on an X-ray?
Signs suggesting a malignant bone lesion in bone lesions radiology might include aggressive periosteal reactions (like a sunburst pattern), cortical destruction, a soft tissue mass, and rapid growth compared to previous imaging.
Can radiology always determine if a bone lesion is cancerous?
While bone lesions radiology can often strongly suggest the nature of a lesion, a definitive diagnosis usually requires a biopsy. The biopsy allows for microscopic examination of the tissue, providing a confirmed diagnosis of whether a lesion is benign or malignant.
Hope this peek into bone lesions radiology helped shed some light! Now go forth and conquer those radiographs. You got this!